We define mental health as how we think, feel, and act. It includes our psychological well-being and emotional health.
We know mental illness such as anxiety or depression can make daily life hard. We also know help works. Therapy, counseling, or medicine can help. Simple steps like self-care, mindfulness, sleep, exercise, and strong support systems build resilience.
Key Takeaways
- Mental health is your cognitive, emotional, and behavioral well‑being that shapes how you think, feel, act, and cope across life stages.
- Mental health lies on a spectrum from flourishing to languishing and is not simply the absence of a diagnosable mental illness.
- Biological, life‑experience, family, community, and societal factors all influence mental health and the risk of developing conditions.
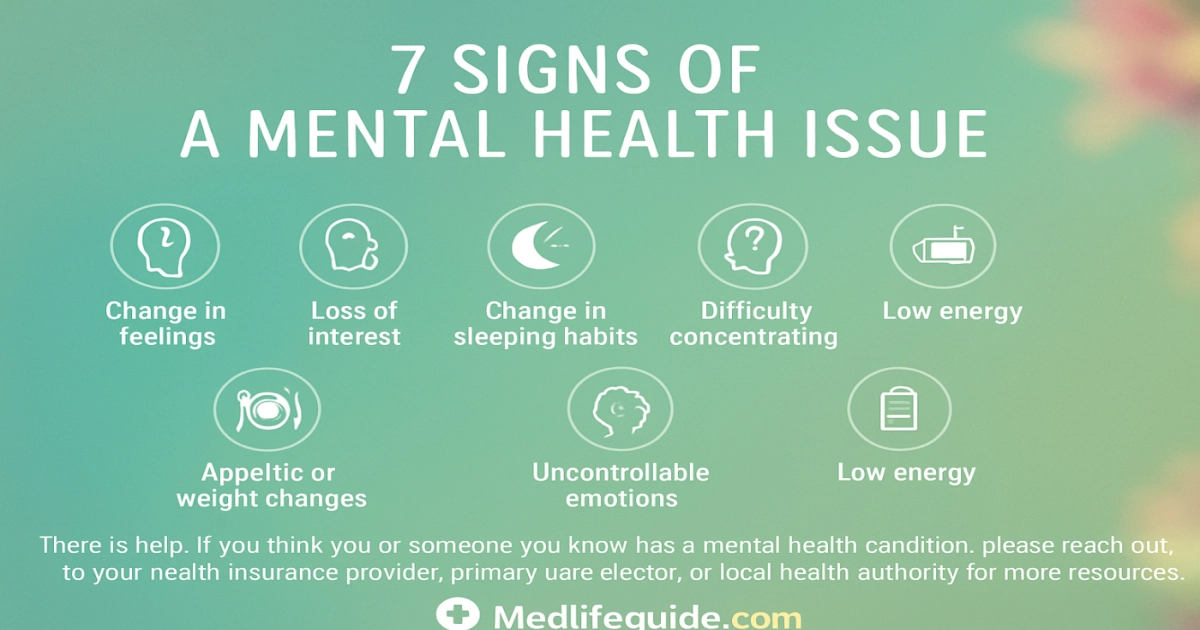
- Early warning signs include major changes in sleep or appetite, withdrawal, low energy, persistent worry or mood swings, unexplained aches, or suicidal thoughts, and recognizing them early improves outcomes.
- Prevention and care—regular self‑care, social connection, accessible professional treatment, and public‑health actions—build resilience and protect both mental and physical health.
Understanding Mental Health and Its Importance

We define mental health as how our mind, feelings and behavior work together so we can learn, connect and cope. It includes psychological well-being, emotional health and cognitive health. Good mental wellness helps at school, with friends and in our physical health. When mental health is poor it can become a mental illness such as depression or anxiety. A psychiatric evaluation or psychotherapy can help diagnose and treat these problems.
- Withdrawing: Losing interest in friends or activities
- Mood changes: Feeling very sad, very angry or having quick mood swings
- Sleep or appetite shifts: Sleeping too much or too little and big changes in eating
- Concentration problems: Finding it hard to focus at school or at home
- Physical complaints: Headaches or stomachaches with no clear cause
- Risky behavior: Using drugs or acting without thinking about danger
- Talk of harm: Saying they want to hurt themselves or others—get help right away
| Sign | What we can do |
|---|---|
| Feeling anxious or sad | Try mindfulness, talk with a trusted adult, or consider therapy |
| Difficulty functioning | See a school counselor, learn stress management techniques and build support systems |
Early support matters: effective counseling, cognitive behavioral therapy or psychiatric care plus family support can change outcomes.
We recommend simple self-care habits: regular sleep, daily activity, balanced food and asking for emotional support. For example, proper eating and hydration help energy, mood and organs such as the kidneys protect kidneys. If symptoms are serious, professionals may offer psychiatric medication and structured treatment. Awareness and resilience help us protect our behavioral health and grow in school, friendships and life.
Sign 1: Persistent Sadness or Low Mood

Persistent sadness or low mood that lasts most days for weeks is a clear early sign our mental health and emotional health need attention. When it affects sleep, schoolwork or friendships we must act. Small changes at initial can become bigger problems if we ignore them.
- Low energy: You may feel tired even after rest which can lower concentration and grades.
- Loss of interest: Hobbies and friends seem less fun and you might spend more time alone.
- Physical changes: Appetite or sleep may shift, there may be unexplained aches, or movements may seem slower.
- Hopeless thoughts: Persistent negative thoughts can signal a mood disorder like depression.
| Symptom | What We Can Do |
|---|---|
| Persistent sadness | Talk with a trusted adult, see a school counselor, consider therapy or counseling. |
| Dropping grades / isolation | Use stress management and mindfulness and build a support system. |
Take early steps: speak with a parent or school nurse and ask for a psychiatric evaluation if needed. Explore evidence-based options such as cognitive behavioral therapy, psychotherapy or when prescribed psychiatric medication. Combining self-care, exercise, sleep hygiene and social emotional support helps build psychological resilience. You can also read about prevention and treatments.
A persistent low mood is not a character flaw; it is a medical signal that effective help, counseling, therapy and community support can address. CDC, WHO
Stay alert to stigma and speak up for mental health awareness so everyone can get timely care for anxiety, mood disorders and other mental disorders.
Sign 2: Excessive Worry or Anxiety

Excessive worry or anxiety happens when thoughts run nonstop and make it hard to sleep, finish schoolwork, or be with friends. You will notice this sign when normal stress becomes constant and starts to get in the way of daily life. It can be an early sign of a mental disorder like generalized anxiety disorder and may co-occur with depression. Sometimes the worry builds slowly. Other times it seems to appear out of nowhere.
- Physical signs: A fast heartbeat, stomach aches, or headaches that come with worry.
- Behavioral signs: Avoiding tests, skipping friends, or not trying new things to stop the worry.
- Cognitive signs: Saying “what if” over and over, trouble focusing, and reduced cognitive function.
Try practical steps initial. Use mindfulness, paced breathing, better sleep hygiene and peer support systems to lower stress. Before a test, a few slow breaths can help you focus. If worry becomes severe, research supports cognitive behavioral therapy and a psychiatric evaluation. Sometimes psychiatric medication with therapy helps restore psychological well being.
| Common Worry | When to Seek Help |
|---|---|
| Short episodes tied to events | Daily, intense worry that limits activities |
When worry limits school or friendships, reach out to a trusted adult and consider counseling. Early action builds psychological resilience.
- Talk: Tell a parent, teacher, or counselor.
- Act: Try stress management and self-care, or see a provider for therapy or treatments.
Sources: CDC, WHO, APA research on anxiety and treatment effectiveness. See thyroid nodules.
Sign 3: Changes in Sleep Patterns

Changes in sleep patterns often signal shifts in mental health and emotional well-being. We should treat them as early warning signs of anxiety, depression or other mood disorders.
- Trouble falling or staying asleep: Losing sleep raises stress and can make anxiety worse or trigger panic. For example, poor sleep before a big test can make concentration and calm harder to find.
- Sleeping too much: Hypersomnia can be a sign of depression or low energy linked to some mental disorders. You may sleep through the day or struggle to get moving.
- Irregular sleep schedule: Waking at night or a reversed sleep routine may reflect trauma, poor sleep hygiene or medication effects. Staying up all night and trying to sleep during daytime can affect school and mood.
If sleep changes last two weeks or more we act sooner. Early action supports recovery and builds psychological resilience.
| Change | May indicate |
|---|---|
| Difficulty sleeping | Heightened anxiety, stress or stimulant use |
| Oversleeping | Possible depression or low activity |
We recommend practical steps: maintain a routine, practice mindfulness and self-care, limit screens before bed and reach out to trusted adults or support systems. If sleep problems persist seek therapy, counseling or a psychiatric evaluation to explore diagnosis and treatment options such as cognitive behavioral therapy or psychiatric medication. CDC guidance on sleep and mental health
Sign 4: Withdrawal from Social Activities

Withdrawal from social activities is an early sign that our mental health or emotional health may be affected. When friends, hobbies or family invitations are refused again and again, pay attention to possible depression, anxiety or other mental disorders.
- Avoidance: Skipping clubs or refusing to hang out may show low energy or social anxiety.
- Silent changes: Talking less and spending more time alone could signal mood problems or too much stress.
- Decline in performance: Falling grades or a loss of interest in activities often happen with social withdrawal and other changes in thinking or behavior.
Try these concrete steps:
- Reach out: Talk calmly and listen. Emotional support from friends or family builds psychological resilience.
- Seek help: Encourage a school counselor, therapy or counseling and, if needed, a psychiatric evaluation to learn about treatments like CBT or psychiatric medication.
- Practice self-care: Use mindfulness, regular sleep, exercise and stress management to support mental wellness.
| Behavior | What it may mean / Next step |
|---|---|
| Refuses invitations | Check for anxiety or low mood; offer to join them and suggest a trusted adult or counseling. |
| Stops hobbies | Talk about possible stressors; consider therapy, support from others and stress management techniques. |
We must treat social withdrawal as a sign not a choice. Early support, mental health awareness and access to mental healthcare improve outcomes. CDC, NIMH
Sign 5: Difficulty Concentrating or Making Decisions
Difficulty concentrating or having trouble making choices is an early sign that mental and emotional health need attention. Notice these changes early so you can get help sooner.
When focus fades in class, school work takes much longer, or small decisions like what to eat or who to sit with feel overwhelming, the cause is often stress, anxiety or depression. These problems change how we feel and think. They can lower school performance and make it harder to connect with friends.
- School focus drops: Missed details and incomplete tasks
- Slow decisions: Everyday choices feel confusing or scary
- Memory slips: Forgetting steps or losing track of thoughts
Key: Difficulty concentrating can be a symptom of mood disorders or other mental disorders. It often improves with mindfulness, self-care, counseling or cognitive behavioral therapy.
- Talk to an adult: Share how you feel with a parent, teacher or school counselor
- Try skills: sleep hygiene, short mindfulness breaks and structured routines, and consider healthy foods
- Get professional help: see your primary care provider for evaluation, or ask about therapy and psychiatric medication if needed
| When to seek help | Who to contact |
|---|---|
| Symptoms last longer than 2 weeks or harm daily life | Parent, school counselor or mental health services |
| Thoughts of hurting yourself or others | Emergency services or crisis line (988) |
We encourage mental health awareness and building strong support systems and psychological resilience so young people can return to learning, playing and thriving. With the right support, most students get better and feel more like themselves again.
Sign 6: Changes in Appetite or Weight
A steady change in appetite or weight can be an early sign that our mental health or psychological well-being is affected.
We often see two patterns: unexplained weight loss and eating less, often linked to anxiety or depression, and increased appetite or weight gain, which can happen with some mood disorders or as a side effect of psychiatric medication. Rapid changes that make it hard to do school work, sleep well or keep friends need attention and a mental health assessment.
Act early: small, tracked changes in eating can point to helpful steps like therapy, counseling or medical review.
- Track changes: Record meals, mood and sleep so you can spot patterns.
- Talk to adults: Tell a parent, teacher or school nurse when appetite shifts.
- Seek professional help: Consider psychiatric evaluation, CBT or medication advice when needed.
| Change | Possible link |
|---|---|
| Loss of appetite / weight loss | anxiety, depression and stress |
| Increased appetite / weight gain | mood disorders, medication side effects and emotional eating |
Try self-care, mindfulness and leaning on support systems while you arrange professional guidance from a psychologist or psychiatrist to clarify diagnosis and treatment. Look after your body too, for example staying hydrated and learning about kidney health.
Sign 7: Feelings of Hopelessness or Worthlessness
Sign 7: Feelings of Hopelessness or Worthlessness: This happens when someone believes nothing will get better and that they have little value. These feelings are key signs of depression and can appear with anxiety, mood disorders or other mental disorders. They affect emotional health, daily activities and school work; biological factors, stress and trauma can all reduce psychological well-being1.
What we can do immediately:
- Talk to someone: Tell a trusted adult or friend about your feelings.
- Use self-care: Good sleep, healthy food, regular activity and mindfulness can help your mood.
- Seek help: Ask for counseling, school support or a psychiatric evaluation.
- Try therapy options: cognitive behavioral therapy and psychotherapy can rebuild psychological resilience.
| Sign | Immediate action |
|---|---|
| Feeling worthless or helpless | Tell a caregiver; access mental health services or your school counselor |
| Persistent hopeless thoughts | Ask for an evaluation; consider therapy or medical treatment if recommended |
Treat hopelessness as a signal: timely support, social support and professional care can restore mental wellness.
If feelings persist, contact a provider for mental health assessment, discuss psychiatric medication if needed and create a plan with support systems and stress management.
1Evidence links persistent hopelessness to increased risk of depression and reduced functioning (CDC, 2024).
The Role of Therapy and Counseling in Mental Health
Mental health matters for how we think, feel and act. Therapy and counseling are powerful tools that protect our psychological well-being and emotional health.
We use psychotherapy to talk through problems, build resilience, and learn skills for stress management, mindfulness and self-care. When symptoms point to a mental illness, such as severe anxiety or depression or a mood disorder, we pair counseling with clinical steps like medical evaluation and when needed psychiatric medication. This combined approach helps people feel safer and make real progress.
- When to seek help: If low mood stays for weeks, if panic starts to interfere with daily life, or if you have thoughts of self-harm, tell a trusted adult or contact a health provider right away.
- What to expect: A careful assessment, talk therapy, practice of new skills, and referrals for medication or group support when needed.
- How it helps: You learn better ways to cope, symptoms often decrease, and you build stronger support from family, friends and professionals.
Therapy reduces stigma, strengthens support systems and improves mental wellness across childhood, adolescence and adulthood. CDC, WHO
| Therapy type | Main benefits |
|---|---|
| Counseling / Psychotherapy | Emotional support, coping skills and stress management |
| Cognitive Behavioral Therapy (CBT) | Helps change unhelpful thoughts and reduces anxiety and depression |
| Psychiatric assessment / treatment | Provides diagnosis, medication management and coordinated care |
Importance of Support Systems for Mental Well-being
Strong support systems protect our mental health. They lower anxiety and depression and build psychological resilience. That makes it easier to handle stress and school challenges.
| Support Type | How it helps |
|---|---|
| Family & Friends | Provide emotional support and help with daily coping. |
| School Counselors / Therapy | Offer counseling, CBT and referrals to psychiatric care. |
| Community & Online Groups | Teach mindfulness, self-care and reduce stigma. |
- Talk to someone: Share feelings with a trusted adult or peer.
- Seek help: Ask for therapy or a psychiatric evaluation if symptoms persist.
- Use tools: Practice stress management, mindfulness and regular self-care.
When we connect we lower risk for mood disorders and strengthen our chances to recover. Treatment and mental health services make a real difference.
Act early. Spot warning signs of mental illness and use emotional support, psychotherapy or psychiatric medication when recommended. Early steps improve outcomes according to CDC and WHO.
Frequently Asked Questions
Mental health is your cognitive, emotional and behavioral well‑being—how you think, feel and act—and it matters since it determines your ability to cope with stress, form relationships, work productively and affects physical health, so prevention and timely care improve quality of life.
Seven common signs to watch for are persistent sadness or hopelessness; severe mood swings or irritability; social withdrawal or loss of interest; changes in sleep or appetite; low energy or trouble concentrating; increased use of alcohol/drugs or risky coping; and thoughts of self‑harm, suicidal ideation, or other alarming symptoms (e.g., hearing voices).
If you notice one or more signs, respond with empathy—ask about safety, listen without judgment, encourage and help connect them (or yourself) to a primary care provider or mental health professional, use crisis resources (call/text 988 or 911 if there’s immediate danger), and support ongoing self-care and follow‑up.