Medically Reviewed and Compiled by Dr. [Adam N. Khan], MD.
LDL cholesterol, commonly referred to as “bad cholesterol,” is one of the most critical and well-studied biomarkers in cardiovascular medicine. Elevated LDL cholesterol is a primary, causal risk factor for atherosclerotic cardiovascular disease (ASCVD), including coronary artery disease, hear
Medically Reviewed and Compiled by Dr. [Adam N. Khan], MD.
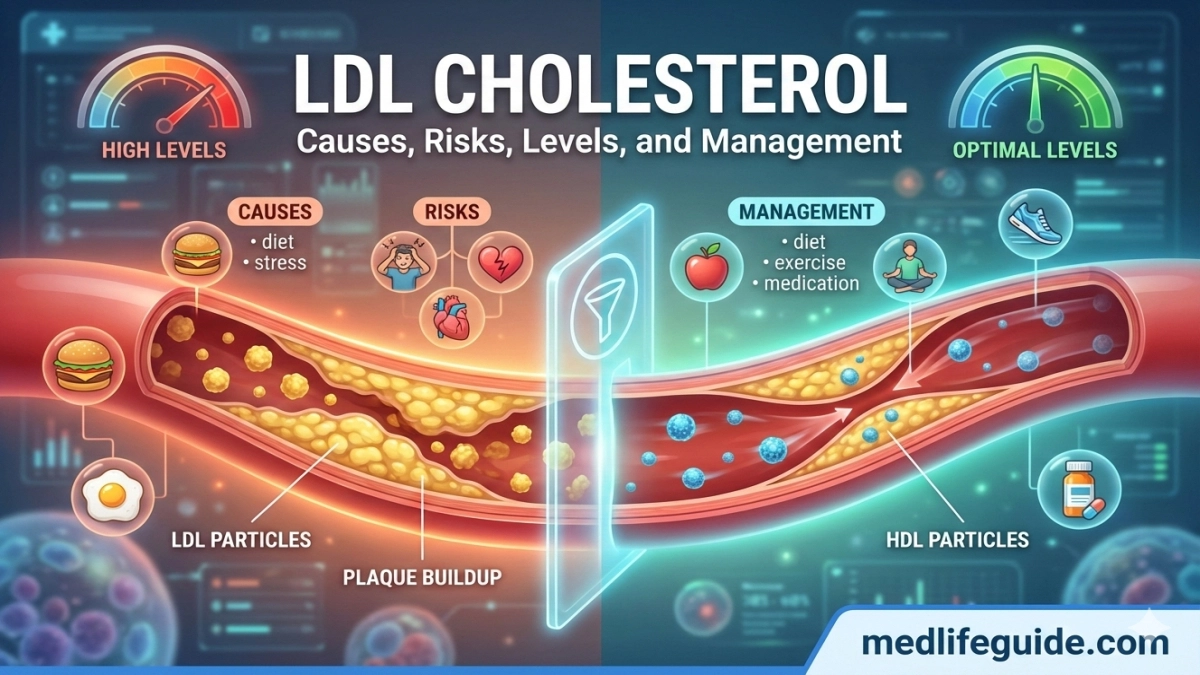
LDL cholesterol, commonly referred to as “bad cholesterol,” is one of the most critical and well-studied biomarkers in cardiovascular medicine. Elevated LDL cholesterol is a primary, causal risk factor for atherosclerotic cardiovascular disease (ASCVD), including coronary artery disease, heart attack, and ischemic stroke. Despite its widespread recognition, LDL cholesterol is often misunderstood by patients and even underestimated in long-term risk assessment.
This article provides a comprehensive, evidence-based explanation of LDL cholesterol, including its biological role, normal and abnormal levels, causes of elevation, health consequences, diagnostic strategies, and modern treatment approaches. Special emphasis is placed on nuanced clinical considerations and patient-centered insights that go beyond basic definitions.
What Is LDL Cholesterol?
LDL stands for low-density lipoprotein. It is one of several particles that transport cholesterol through the bloodstream. Cholesterol itself is a waxy, fat-like substance essential for hormone production, cell membrane integrity, and vitamin D synthesis.
How LDL Cholesterol Works
- LDL particles carry cholesterol from the liver to peripheral tissues.
- When LDL levels are excessive, cholesterol can deposit in arterial walls.
- This process initiates and accelerates atherosclerosis, the buildup of plaques inside arteries.
LDL cholesterol is measured in milligrams per deciliter (mg/dL) through a standard blood lipid panel.
Why LDL Cholesterol Is Considered “Bad”
LDL cholesterol earns its “bad” label because of its direct role in plaque formation.
LDL and Atherosclerosis
- LDL particles penetrate the inner lining of arteries.
- They undergo oxidation and trigger inflammatory responses.
- Immune cells engulf oxidized LDL, forming foam cells.
- Over time, plaques narrow arteries and reduce blood flow.
Plaque rupture can cause sudden clot formation, leading to heart attack or stroke.
Normal, Borderline, and High LDL Cholesterol Levels
LDL cholesterol targets vary based on individual cardiovascular risk.
Standard LDL Cholesterol Ranges
- Optimal: <100 mg/dL
- Near optimal: 100–129 mg/dL
- Borderline high: 130–159 mg/dL
- High: 160–189 mg/dL
- Very high: ≥190 mg/dL
For high-risk individuals (existing heart disease, diabetes, or multiple risk factors), guideline-recommended targets are often below 70 mg/dL.
Causes of High LDL Cholesterol
Elevated LDL cholesterol typically results from a combination of genetic, dietary, metabolic, and lifestyle factors.
Dietary Contributors
- High intake of saturated fats (red meat, butter, full-fat dairy)
- Trans fats (processed and fried foods)
- Excess dietary cholesterol in susceptible individuals
Lifestyle Factors
- Physical inactivity
- Obesity, particularly central obesity
- Tobacco use
- Excessive alcohol consumption
Medical and Genetic Causes
- Familial hypercholesterolemia
- Hypothyroidism
- Type 2 diabetes mellitus
- Chronic kidney disease
- Certain medications (e.g., corticosteroids)
Health Risks Associated With High LDL Cholesterol
Persistently elevated LDL cholesterol significantly increases long-term morbidity and mortality.
Cardiovascular Complications
- Coronary artery disease
- Myocardial infarction
- Ischemic stroke
- Peripheral artery disease
Systemic Effects
- Reduced arterial elasticity
- Endothelial dysfunction
- Chronic vascular inflammation
Large-scale studies confirm a dose-dependent relationship between LDL cholesterol levels and cardiovascular event risk.
How LDL Cholesterol Is Diagnosed
LDL cholesterol is primarily assessed through a fasting or non-fasting lipid panel.
Components of a Lipid Panel
- Total cholesterol
- LDL cholesterol
- HDL cholesterol
- Triglycerides
Calculated vs. Direct LDL
- Most labs calculate LDL using the Friedewald equation.
- Direct LDL measurement is used when triglycerides are very high.
Regular screening is recommended for adults, with earlier testing for those with risk factors or family history.
Treatment and Management of High LDL Cholesterol
Management strategies are individualized based on absolute cardiovascular risk.
Lifestyle-Based Interventions
- Mediterranean or DASH-style diets
- Increased soluble fiber intake
- Regular aerobic exercise
- Weight reduction
- Smoking cessation
Pharmacological Treatments
- Statins: First-line therapy; reduce LDL and cardiovascular events
- Ezetimibe: Reduces intestinal cholesterol absorption
- PCSK9 inhibitors: Injectable agents for high-risk or statin-intolerant patients
- Bempedoic acid: Oral option for statin intolerance
Treatment decisions follow evidence-based clinical guidelines and shared decision-making.
LDL Cholesterol in Special Populations
LDL Cholesterol and Diabetes
Patients with diabetes have higher baseline cardiovascular risk, even with modest LDL elevations. Aggressive LDL lowering is standard in this group.
LDL Cholesterol in Older Adults
Chronological age alone does not negate benefit from LDL reduction. Functional status and comorbidities guide treatment intensity.
LDL Cholesterol in Familial Hypercholesterolemia
This genetic condition causes lifelong elevated LDL cholesterol and requires early, aggressive therapy.
Unique Clinical Takeaways
1. LDL Particle Number vs. LDL Concentration
Standard LDL cholesterol measures cholesterol content, not particle count. Some patients with “normal” LDL levels still have high LDL particle numbers, increasing cardiovascular risk. Advanced lipid testing can refine risk stratification in select cases.
2. Inflammation Modulates LDL Risk
LDL cholesterol is more harmful in the presence of systemic inflammation. Patients with elevated inflammatory markers may experience cardiovascular events at lower LDL levels, supporting aggressive prevention strategies.
3. Patient Adherence Outweighs Drug Potency
Clinical outcomes are often determined more by long-term adherence than by choosing the strongest medication. Simplified regimens, education, and addressing side-effect concerns significantly improve LDL control and outcomes.
LDL Cholesterol Myths and Misconceptions
“Diet Alone Can Always Normalize LDL”
Dietary changes are effective but insufficient for many high-risk or genetically predisposed patients.
“High LDL Doesn’t Matter Without Symptoms”
Atherosclerosis progresses silently for decades. Symptoms often appear only after significant damage.
“Statins Are Dangerous”
Extensive data show statins are generally safe, with serious adverse effects being uncommon and reversible.
Monitoring and Long-Term Follow-Up
LDL cholesterol should be rechecked:
- 4–12 weeks after therapy initiation or change
- Every 3–12 months once stable
Long-term management focuses on sustained LDL reduction rather than short-term fluctuations.