Medically Reviewed and Compiled by Dr. Adam N. Khan, MD.
Stress is a universal human experience—but chronic, unmanaged, or overwhelming stress can significantly distort how the brain functions, how emotions are regulated, and how a person behaves in daily life. Understanding the key signs of stress affecting mental health is not just helpful for early detection—it’s essential for preventing long-term psychological and physiological complications.
This in-depth medical guide explores the full symptom spectrum, the neurobiology behind stress, real-life examples from clinical practice, and unique clinical insights that most traditional wellness articles don’t cover.
The Physiology of Stress: How It Disrupts Mental Health
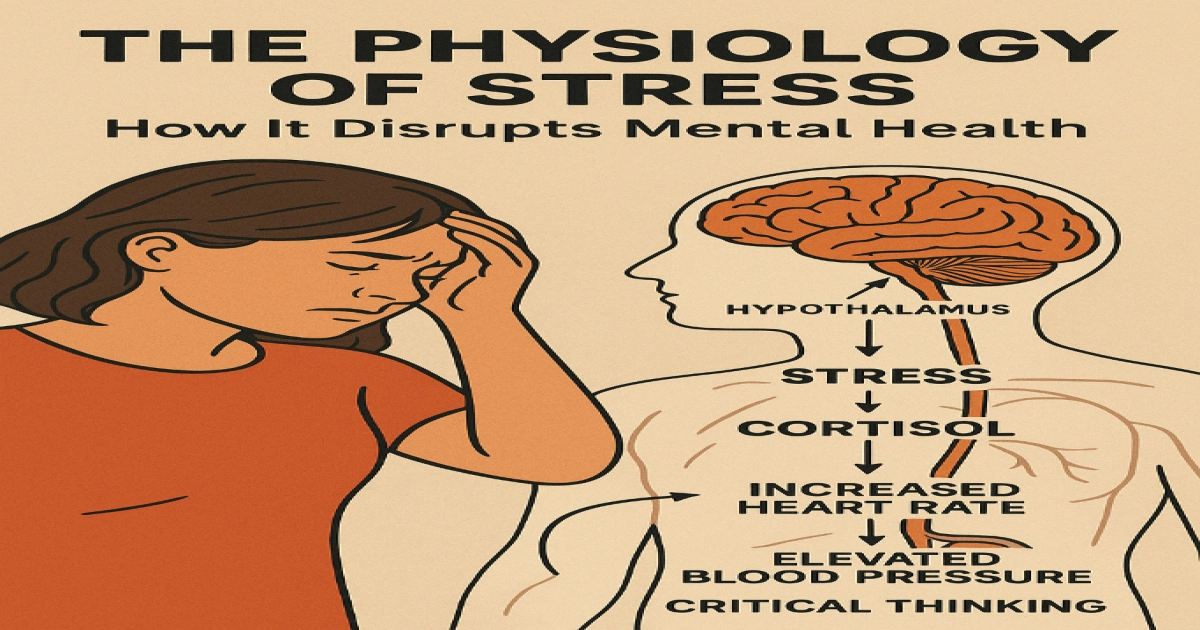
When the brain perceives a threat—emotional, physical, or psychological—it activates the hypothalamic-pituitary-adrenal (HPA) axis, increasing cortisol and adrenaline production.
Short bursts of stress help survival.
Chronic stress rewires the brain, specifically:
- Shrinks the prefrontal cortex (affects decision-making, focus, emotional control)
- Enlarges and overstimulates the amygdala (increasing fear, anxiety, and irritability)
- Disrupts serotonin, dopamine, and norepinephrine levels
- Interferes with sleep architecture
- Weakens the immune system and gut-microbiome balance
Over time, these changes translate into emotional, cognitive, behavioral, and physical symptoms.
Key Signs of Stress Affecting Mental Health
Below is a comprehensive overview of how stress manifests across different aspects of mental and emotional well-being.
Emotional and Psychological Signs
1. Persistent Anxiety or Excessive Worry
Chronic stress causes the amygdala to remain hyperactive, creating a continuous sense of danger or unease.
Real-life example:
A patient working in tech began experiencing constant “what if” thinking during layoffs—not just at work, but even during family meals or rest time.
2. Irritability, Anger, or Emotional Volatility
Stress lowers frustration tolerance, making small inconveniences feel overwhelming.
3. Low Mood or Depressive Symptoms
Constant cortisol exposure reduces serotonin activity, leading to:
- Emotional numbness
- Loss of joy
- Increased sadness
4. Feeling Overwhelmed
Simple tasks may feel unmanageable, signaling a decline in the brain’s executive function.
5. Withdrawal or Detachment
People sometimes isolate themselves because interacting feels mentally taxing.
Cognitive Signs
1. Brain Fog & Difficulty Concentrating
The prefrontal cortex becomes less active, causing:
- Forgetfulness
- Reduced processing speed
- Difficulty multitasking
2. Racing Thoughts
Stress can trigger mental hyperactivity that feels uncontrollable.
3. Indecisiveness
Even simple decisions—like what to eat—may feel draining.
4. Negative or Intrusive Thinking
Stress amplifies rumination and worst-case scenario thinking.
Behavioral Signs
1. Avoidance Behaviors
Individuals may avoid:
- Social gatherings
- Work tasks
- Conversations
- Decision-making responsibilities
2. Changes in Eating Habits
Both overeating (comfort seeking) and appetite loss are common.
3. Sleep Problems
Stress impairs melatonin production and raises cortisol, causing:
- Trouble falling asleep
- Frequent waking
- Nighttime anxiety
- Vivid stress-related dreams
4. Increased Reliance on Coping Mechanisms
This may include:
- Coffee multiple times a day
- Alcohol to unwind
- Smoking
- Excessive screen time
- Overworking as a distraction
Physical Signs (Mind–Body Connection)
1. Headaches or Tension Migraines
Stress-induced muscle tightening of the neck and scalp contributes significantly.
2. Digestive Issues
The gut-brain axis is deeply connected:
- Nausea
- IBS flares
- Bloating
- Acid reflux
- Constipation or diarrhea
3. Muscle Pain or Body Aches
Prolonged tension can lead to chronic pain in:
- Neck
- Back
- Jaw (TMJ)
4. Fatigue or Low Energy
Even after sleeping, the person may feel exhausted.
5. Heart Palpitations or Rapid Heart Rate
Often misinterpreted as heart disease.
Real-life clinical case example:
A 32-year-old woman repeatedly visited ER for chest tightness. ECGs were normal. Eventually diagnosed with stress-induced panic disorder.
Unique Clinical Takeaways
These insights reflect deeper clinical realities rarely mentioned in standard online articles.
1. Stress Frequently Mimics Other Mental Health or Medical Disorders
Stress symptoms overlap with:
- ADHD (inattention, restlessness)
- Hypothyroidism (fatigue, cognitive decline)
- Hormonal imbalance
- GAD and panic disorder
- Depression
Why this matters:
Misdiagnosis leads to incorrect treatment.
Clinicians must carefully analyze:
- Onset timeline
- Symptom patterns
- Life stressors
- Sleep cycles
- Occupational or family pressures
Stress is a diagnosis of context, not just symptoms.
2. High-Functioning Individuals Often Miss Early Warning Signs
People who excel under pressure—healthcare workers, IT professionals, caregivers, entrepreneurs—may not recognize early signs because stress has become normalized.
Subtle indicators unique to this group:
- Working late even when tired
- Feeling guilty during rest
- Thinking about work 24/7
- Difficulty relaxing during weekends
- Using productivity as validation
These patients often present with advanced burnout rather than mild stress.
3. Stress Symptom Clusters Predict Severity More Accurately Than Individual Symptoms
Doctors often look for clusters for early intervention:
Cluster 1: Sleep Issues + Anxiety + GI Problems
Indicates early autonomic dysfunction.
Cluster 2: Fatigue + Emotional Numbness + Cognitive Decline
Suggests burnout or early depressive symptoms.
Cluster 3: Irritability + Overworking + Social Withdrawal
Common in high-pressure professionals.
Recognizing clusters helps prevent escalation into:
- Panic disorder
- Major depressive disorder
- Severe burnout
- Substance misuse
When to Seek Professional Help
See a healthcare professional if you experience:
- Symptoms lasting more than 4–6 weeks
- Difficulty performing daily tasks
- Persistent sleep disturbance
- Panic attacks
- Loss of interest in activities
- Feeling emotionally detached
- Substance use to cope
- Thoughts of hopelessness
Emergency help is essential if there are any thoughts of self-harm or suicide.
Evidence-Based Strategies to Manage Stress
1. Cognitive Behavioral Therapy (CBT)
CBT helps patients identify distorted thought patterns and reframe them effectively.
2. Mindfulness and Breathwork
These techniques reduce autonomic hyperarousal.
3. Exercise
20–30 minutes of moderate aerobic exercise reduces cortisol and enhances dopamine.
4. Sleep Optimization
Improving circadian rhythm through:
- Consistent bedtimes
- Reduced screen time
- Limiting caffeine after noon
5. Social Support
Talking to trusted people reduces emotional burden.
6. Nutrition and Hydration
Anti-inflammatory foods support brain function and help regulate cortisol.
7. Setting Boundaries
Saying no and reducing workload are essential for recovery.
Real-Life Examples of Stress Impact
Here are realistic scenarios often seen in clinical practice:
Case Example 1: The Overworked Parent
A single mother juggling work and childcare reported:
- Forgetting appointments
- Nighttime worry
- Emotional exhaustion
Diagnosis: Chronic stress leading to adjustment disorder
Case Example 2: The High-Pressure Student
A medical student experienced:
- Panic attacks before exams
- Memory issues
- GI symptoms
Intervention: CBT + sleep therapy.
Case Example 3: The Corporate Professional
A 45-year-old executive reported:
- Heart palpitations
- Anger outbursts
- Poor sleep
Diagnosis: Stress-induced anxiety disorder.
These examples showcase how stress manifests differently based on lifestyle, personality, and responsibilities.
FAQs About Stress and Mental Health
Chronic stress can cause long-lasting brain changes, but many are reversible with treatment and lifestyle intervention.
Yes. Stress affects digestion, sleep, immunity, and muscle tension through the brain-body connection.
Yes. Overactivation of the amygdala creates intense fear, overwhelm, and panic sensations.
Recovery depends on severity. Mild cases may improve in weeks; severe burnout may take months.
Medical Disclaimer
This content is for educational purposes only and should not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for personalized medical guidance.

