Medically Reviewed and Compiled by Dr. Adam N. Khan, MD.
Why Colon Cancer Screening is Your Best Defense
Colon cancer is a unique health challenge because it is one of the most preventable types of cancer. Unlike many other illnesses that only show up once they have caused significant damage, colon cancer often starts as small, non-cancerous growth
Medically Reviewed and Compiled by Dr. Adam N. Khan, MD.
Why Colon Cancer Screening is Your Best Defense
Colon cancer is a unique health challenge because it is one of the most preventable types of cancer. Unlike many other illnesses that only show up once they have caused significant damage, colon cancer often starts as small, non-cancerous growths called polyps.
Screening is the process of finding these polyps before they turn into cancer.
When we talk about “screening,” we aren’t just talking about a medical check-up. We are talking about a proactive way to stop a disease in its tracks. In 2026, the medical community has shifted its focus heavily toward early detection because the data is clear: when caught early, the survival rate for colon cancer is incredibly high.
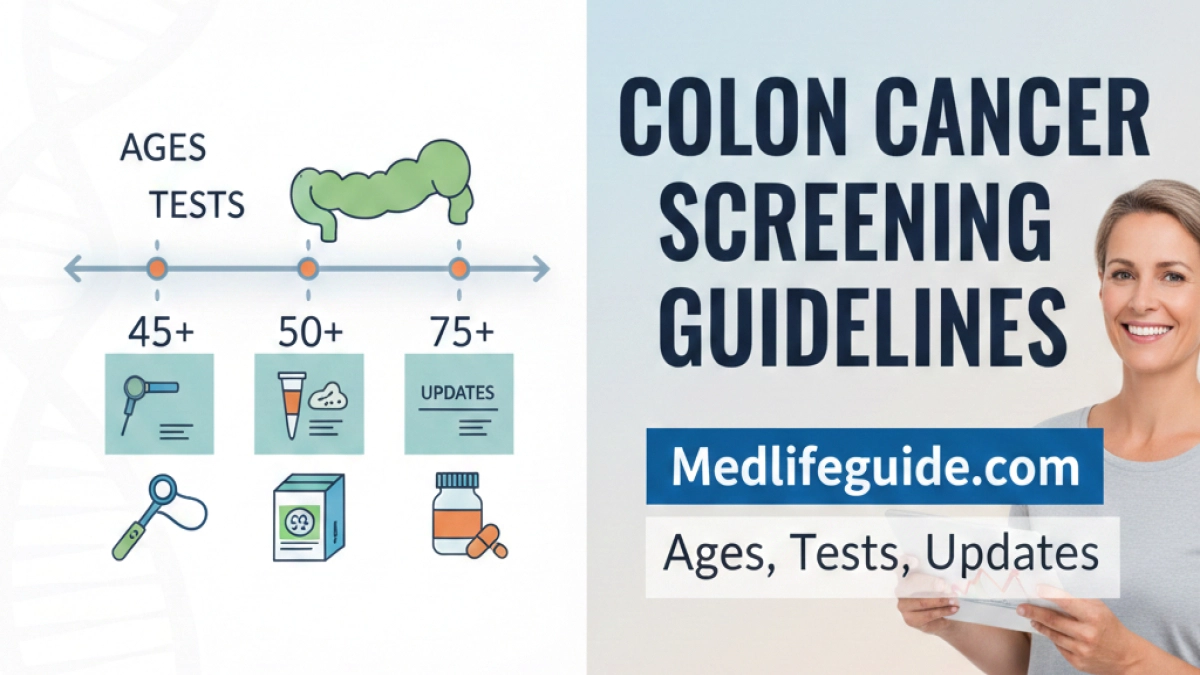
The Shift to Age 45
For years, the standard advice was to start screening at age 50. However, recent trends have shown an increase in colon cancer cases among younger adults. Because of this, leading health organizations now recommend that people at average risk begin regular screening at age 45.
If you have a family history of the disease or certain digestive conditions, your doctor might suggest starting even earlier. This change is vital because it addresses the reality of how this disease is evolving in the modern world.
Understanding Your Screening Options
Many people avoid screening because they think a colonoscopy is the only option. While a colonoscopy is considered the “gold standard,” there are actually several ways to get screened. The best test is the one that actually gets done.
1. Visual Exams (The Structural Approach)
These tests allow a doctor to look inside the colon to find and often remove polyps.
- Colonoscopy: This is the most thorough method. A doctor uses a thin, flexible tube with a camera to examine the entire colon. If they find a polyp, they can remove it right then and there. This makes it both a screening tool and a prevention tool. Usually, if results are clear, you only need one every 10 years.
- CT Colonography (Virtual Colonoscopy): This uses X-rays and computers to produce images of the colon. It is less invasive than a traditional colonoscopy, but if something is found, a regular colonoscopy will still be needed to remove it.

2. Stool-Based Tests (The At-Home Approach)
These tests look for signs of cancer or polyps in the stool. They are non-invasive and can be done in the privacy of your own home.
- FIT (Fecal Immunochemical Test): This test looks for hidden blood in the stool, which can be an early sign of polyps or cancer. It needs to be done every year.
- MT-sDNA (Stool DNA Test): This test looks for both blood and specific DNA changes associated with cancer. This is usually done every three years.
| Test Type | Frequency | Main Benefit |
| Colonoscopy | Every 10 years | Can remove polyps during the test. |
| FIT Test | Every year | No prep required; done at home. |
| Stool DNA | Every 3 years | Highly sensitive for finding cancer. |
What to Expect During a Colonoscopy
The word “colonoscopy” often makes people nervous, but the process is much simpler than most people imagine. Understanding the steps can help remove the “fear of the unknown.”
The Preparation Phase
The day before the procedure is the most important part. You will need to follow a clear liquid diet and take a special laxative solution to “prep” or clean out your colon. A clean colon allows the doctor to see the lining clearly. While the prep isn’t the most fun part of the week, it is the key to an accurate exam.
The Procedure Day
On the day of the test, you are usually given a sedative. Most patients fall into a light sleep and don’t feel a thing. The entire process typically takes about 30 to 60 minutes. Because of the sedation, you’ll need a friend or family member to drive you home.
The Recovery
Most people feel back to normal by the next morning. You can usually return to your regular diet immediately. If the doctor removed any polyps, they will send them to a lab to be checked, and you’ll get those results within a week or two.
Risk Factors: Who Needs to Be More Vigilant?
While everyone should be screened starting at 45, some people have a higher risk. If you fall into these categories, you should have a detailed conversation with your healthcare provider.
- Family History: If a parent or sibling has had colorectal cancer or polyps, your risk is higher.
- Race and Ethnicity: African Americans have the highest incidence and mortality rates of colorectal cancer in the United States.
- Personal Health History: If you have Type 2 diabetes or inflammatory bowel diseases like Crohn’s or Ulcerative Colitis, your risk increases.
- Lifestyle Factors: Diets high in processed meats, smoking, heavy alcohol use, and a sedentary lifestyle are all linked to higher rates of the disease.
Common Myths vs. Facts
To make the best decision for your health, you need the right information. Let’s clear up some common misconceptions.
Myth: “I don’t have symptoms, so I don’t need a screening.”
Fact: This is the most dangerous myth. Colon cancer often has no symptoms in its early stages. Screening is designed to find it before symptoms appear.
Myth: “The procedure is painful.”
Fact: With modern sedation, the vast majority of patients feel no pain during a colonoscopy and have no memory of the procedure afterward.
Myth: “Screening is too expensive.”
Fact: Most insurance plans and Medicare cover colon cancer screening as a preventive service. In many cases, there is little to no out-of-pocket cost.
How to Lower Your Risk Beyond Screening
While screening is the most effective tool, you can also make lifestyle choices that support your colon health.
- Eat Your Fiber: Focus on whole grains, fruits, and vegetables. Fiber helps move waste through your system and keeps the lining of your colon healthy.
- Watch the Red Meat: Try to limit processed meats like deli meats, hot dogs, and sausages, which have been linked to increased cancer risk.
- Stay Active: Regular exercise helps maintain a healthy weight and lowers inflammation in the body.
- Stop Smoking: Smoking isn’t just bad for your lungs; it increases the risk of many cancers, including those of the digestive tract.
Taking the Next Step
Thinking about cancer can be scary, but colon cancer screening is actually an empowering tool. It gives you the power to prevent a major illness before it can ever take hold.
If you are 45 or older, or if you have symptoms like persistent changes in bowel habits, abdominal pain, or blood in your stool, don’t wait. Schedule a consultation with your doctor to discuss which screening method is right for your lifestyle and medical history.
Remember, the goal of screening isn’t just to find cancer—it’s to prevent it.