Wrap-up
- Understanding COVID-19 variants is crucial for predicting case trends and guiding public health responses to mitigate their impact.
- Data analysis is essential for tracking COVID-19 cases and formulating predictive models, enabling proactive responses to emerging outbreaks.
- Public health responses, including various mitigation strategies, play a vital role in managing COVID-19 case trends effectively.
Also Read: New COVID Symptoms Chart 2025
Understanding COVID-19 Variants and Their Impact on Case Trends
The emergence of COVID-19 variants has become a critical aspect of understanding the pandemic’s trajectory. Variants arise due to mutations in the virus’s genetic material, which may lead to changes in transmissibility, virulence, or vaccine escape. This variability plays a significant role in public health responses and influences case trends globally.
The Genesis of Variants
Coronaviruses, including SARS-CoV-2, naturally mutate over time. These mutations can occur during replication when the virus spreads from one individual to another. Most mutations are inconsequential, resulting in a virus that behaves similarly to its predecessors; however, some mutations can allow the virus to better evade the immune system or enhance its capacity to spread. Key variants of interest, such as Alpha, Delta, and Omicron, have shown varying degrees of impact on infection rates, severity of disease, and vaccine efficacy.
Classification of Variants
Variants are typically classified into three categories based on their characteristics:
- Variants of Interest (VOIs): These variants demonstrate genetic changes that are likely to affect virus characteristics such as transmissibility or disease severity. They might be associated with unusual clusters of cases.
- Variants of Concern (VOCs): This classification is given to variants that have shown increased transmissibility, more severe disease, reduced effectiveness of treatments or vaccines, or diagnostic challenges. Such variants require heightened surveillance and preventive measures.
- Variants of Consequence (VOCs): These are variants that have demonstrably impacted global public health efforts. This could include variants that significantly change the pandemic’s trajectory in terms of case numbers or health outcomes.
Impact on Case Trends
The emergence of COVID-19 variants leads to fluctuations in case trends that can be understood through various indicators:
Transmissibility
Some variants, particularly the Delta and Omicron variants, have shown higher transmissibility compared to earlier strains. This increase in spread can lead to significant spikes in cases, particularly in unvaccinated populations or among demographics with lower immunity levels. The rapid transmission rates can overwhelm healthcare systems and complicate containment efforts.
Disease Severity
Certain variants may also exhibit potential changes in disease severity. For instance, while some variants may lead to more cases, they can produce milder illness, whereas others might be associated with more severe outcomes. This factor complicates treatment approaches and health policy responses.
Vaccine Efficacy
Variants can impact the efficacy of existing vaccines, leading to discussions on booster doses. Research has indicated that while vaccines remain effective against many variants, their effectiveness may be reduced against certain strains. This has prompted ongoing studies and adaptations in vaccination strategies, including the development of variant-specific vaccines.
Long-term Implications
Understanding variants is crucial for forecasting future case trends. The continuous evolution of the virus may necessitate adjustments in public health policies, including the re-evaluation of vaccination strategies, the implementation of mask-wearing, and social distancing protocols, especially in light of new and emerging variants.
Monitoring and Surveillance
Sustained monitoring and genomic surveillance are essential in tracking the spread and impact of variants. Public health agencies, such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), advocate for robust reporting and genomic sequencing as a means to provide timely information that informs health decisions.
Conclusion – Understanding COVID-19 Variants and Their Impact on Case Trends
Understanding COVID-19 variants is crucial for predicting case trends and guiding public health responses to mitigate their impact.
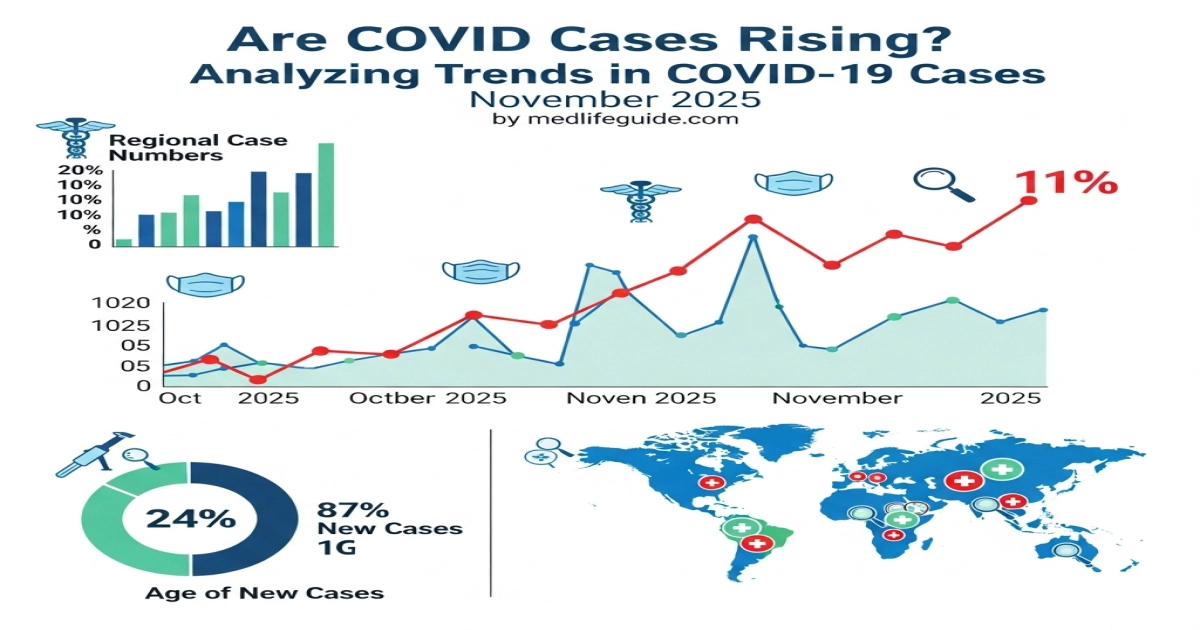
Analyzing Data: Tracking COVID-19 Cases and Predictive Models
The COVID-19 pandemic has underscored the importance of data analysis in public health decision-making. As cases have surged and receded over time, health officials and researchers have relied on accurate and timely data to track infections, inform policy responses, and develop predictive models that can help anticipate future trends. This complex interplay of data collection, analysis, and forecasting can be broken down into several key components.
Data Sources
The reliability of the analysis hinges on the quality of the data collected. Various sources contribute to the data landscape of COVID-19 tracking:
- Government Health Agencies: Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and local health departments provide official case counts, hospitalization statistics, and mortality data, which are critical for tracking the virus’s spread.
- Healthcare Providers: Hospitals and testing centers report their findings, adding granular data that can reflect local outbreaks and the effectiveness of responses.
- Surveys and Mobile Applications: Citizen-reported data through health surveys and symptom tracking apps can fill gaps in official reporting and provide real-time insights into community transmission and individual experiences.
- Academic Research: Universities and research institutions compile and analyze data to understand broader trends, the effectiveness of interventions, and social determinants of health.
Data Analysis Techniques
Once data is collected, it must be processed and analyzed to extract meaningful insights. Key techniques include:
Descriptive Analytics
Descriptive analytics focuses on summarizing historical data to understand the current state of COVID-19. This includes visualizations like:
- Graphs and Charts: Line graphs showing daily case counts can illustrate peaks and valleys in infections. Bar charts can compare cases across regions or demographics.
- Heat Maps: Geographic visualization of COVID-19 cases can highlight hotspots, revealing areas of high transmission risk.
Diagnostic Analytics
Diagnostic analytics goes a step further, looking at correlations and potential causations behind the data. Questions explored include:
- Why are cases rising in specific regions? By analyzing demographic factors, mobility data, and previous health interventions, researchers seek to clarify the causes of spikes.
- What role does vaccination play? By comparing case rates in vaccinated versus unvaccinated populations, analysts glean insights into the efficacy of vaccines in mitigating spread.
Predictive Modeling
Predictive modeling is crucial for anticipating future case trends based on current data. Models utilize statistical techniques and algorithms to project the trajectory of the virus. Key methods include:
SIR Model
The Susceptible-Infectious-Recovered (SIR) model is a fundamental epidemiological model used to predict how a virus might spread over time. The model uses three compartments:
- Susceptible: Individuals at risk of infection.
- Infectious: Those currently infected and capable of spreading the virus.
- Recovered: Individuals who have recovered and are assumed immune.
The interaction of these groups is modeled mathematically to predict the number of new infections and recoveries over time, allowing health officials to forecast healthcare needs and resource allocation.
Machine Learning
More sophisticated techniques often employ machine learning to capture complex patterns in data. Algorithms can analyze thousands of variables, including:
- Demographic information (age, gender, underlying health conditions).
- Mobility data (travel patterns, social distancing behaviors).
- Historical trends (past case surges, seasonal variations).
Machine learning models can improve upon simpler models by constantly learning from new data inputs, thus providing updated predictions as conditions change.
Limitations and Challenges
While data analysis provides invaluable insights, there are several challenges and limitations:
- Data Quality and Availability: Inconsistent reporting, delays, and underreporting can skew data and lead to inaccurate analyses. Efforts must be made to standardize data collection across regions.
- Model Assumptions: Predictive models rely on assumptions regarding human behavior and viral transmission, which can change as new variants emerge or public health measures are implemented. The accuracy of predictions depends on how well these assumptions hold true over time.
- Communication of Uncertainty: Models often come with confidence intervals and ranges. Effectively communicating the uncertainty associated with predictions is vital, as it impacts public perception and policy decisions.
Conclusion – Analyzing Data: Tracking COVID-19 Cases and Predictive Models
Data analysis is essential for tracking COVID-19 cases and formulating predictive models, enabling proactive responses to emerging outbreaks.
Public Health Responses: Mitigation Strategies and Their Effectiveness
Public health responses during the COVID-19 pandemic have been pivotal in controlling the spread of the virus. Understanding these responses, particularly mitigation strategies, involves a comprehensive analysis of their implementation, effectiveness, and the underlying principles guiding public health decision-making.
Mitigation Strategies
Mitigation strategies are actions aimed at reducing the severity and impact of COVID-19. They include a combination of individual and community-level interventions:
1. Social Distancing
Social distancing measures involve maintaining physical space between individuals to minimize virus transmission. These measures have included:
- Closure of non-essential services: Restaurants, gyms, and entertainment venues were temporarily closed or restricted to reduce gatherings.
- Limiting gatherings: Guidelines were established to limit the number of people allowed to congregate in one place.
- Remote work and schooling: Organizations encouraged employees to work from home when possible, and educational institutions shifted to online learning.
2. Mask-Wearing
The widespread adoption of masks has been promoted as a personal protective measure. Masks are effective in preventing respiratory droplets from spreading between individuals. Key aspects include:
- Mandates and recommendations: Governments implemented mask mandates in public spaces, especially indoors or where social distancing was not feasible.
- Public education campaigns: Campaigns aimed to educate the public on the proper use of masks and their role in reducing transmission.
3. Testing and Contact Tracing
Testing and contact tracing are critical components of public health responses:
- Widespread testing: Efforts focused on making testing available to identify and isolate positive cases promptly.
- Contact tracing: Public health officials traced the contacts of confirmed cases to control outbreaks and prevent further spread.
4. Vaccination Campaigns
Vaccination has emerged as a primary long-term strategy to mitigate the effects of COVID-19:
- Development and distribution: Rapid development of vaccines led to campaigns urging vaccination uptake across diverse populations.
- Booster shots: Recommendations for booster doses have been issued to maintain immunity levels, particularly as variants emerged.
5. Quarantine and Isolation
Quarantine and isolation measures are crucial for controlling the spread, particularly for confirmed or suspected cases:
- Isolation of confirmed cases: Individuals who test positive are advised to isolate to prevent infecting others.
- Quarantine of exposed individuals: Those exposed to confirmed cases are asked to quarantine, illustrating the importance of separating potentially infected individuals from the community.
Effectiveness of Mitigation Strategies
The effectiveness of these mitigation strategies can be evaluated through various lenses, such as epidemiological data, healthcare capacity, and social compliance.
1. Epidemiological Impact
Data illustrate that regions implementing stringent mitigation strategies often saw lower rates of COVID-19 transmission compared to areas with relaxed measures. Patterns in case counts, hospitalizations, and mortality rates can be correlated with:
- Timing of interventions: Early implementation of social distancing and mask mandates often yielded better outcomes in terms of controlling spikes in cases.
- Adaptation to changing data: The ability of public health authorities to adjust guidelines based on emerging evidence and local case trends has been crucial.
2. Healthcare System Resilience
Effective mitigation not only impacts infection rates but also influences healthcare systems:
- Preventing surges: By flattening the curve, strategies aimed to prevent overwhelming healthcare systems, allowing for better management of resources and care for patients.
- Impact on other health services: The balance between COVID-19 response and maintaining other essential health services is an ongoing consideration. Well-executed mitigation measures have allowed healthcare systems to cope with increased demand without neglecting other health needs.
3. Public Compliance and Behavioral Factors
The success of mitigation strategies is also dependent on public compliance and behavior change:
- Community engagement: Public trust and compliance are heightened through transparent communication and community involvement in health initiatives. Misinformation and backlash can undermine these efforts.
- Equity and accessibility: Consideration of social determinants of health plays a critical role. Strategies that neglect vulnerable populations may fail to achieve desired outcomes, emphasizing the importance of equitable access to testing, vaccines, and health education.
4. Long-term Considerations
The ongoing evaluation of mitigation strategies extends beyond immediate public health. Long-term societal impacts, such as shifts in work culture, mental health, and economic stability, can influence future health policy and preparedness for pandemics.
Conclusion – Public Health Responses: Mitigation Strategies and Their Effectiveness
Public health responses, including various mitigation strategies, play a vital role in managing COVID-19 case trends effectively.