Quick Summary
Life after a kidney transplant depends heavily on disciplined follow-up care. This includes regular clinic visits, lifelong immunosuppressive medication, routine lab monitoring, and informed lifestyle changes. With proper follow-up, one-year graft survival now exceeds 95% in many centers. The keys to long-term success include medicatio
Quick Summary
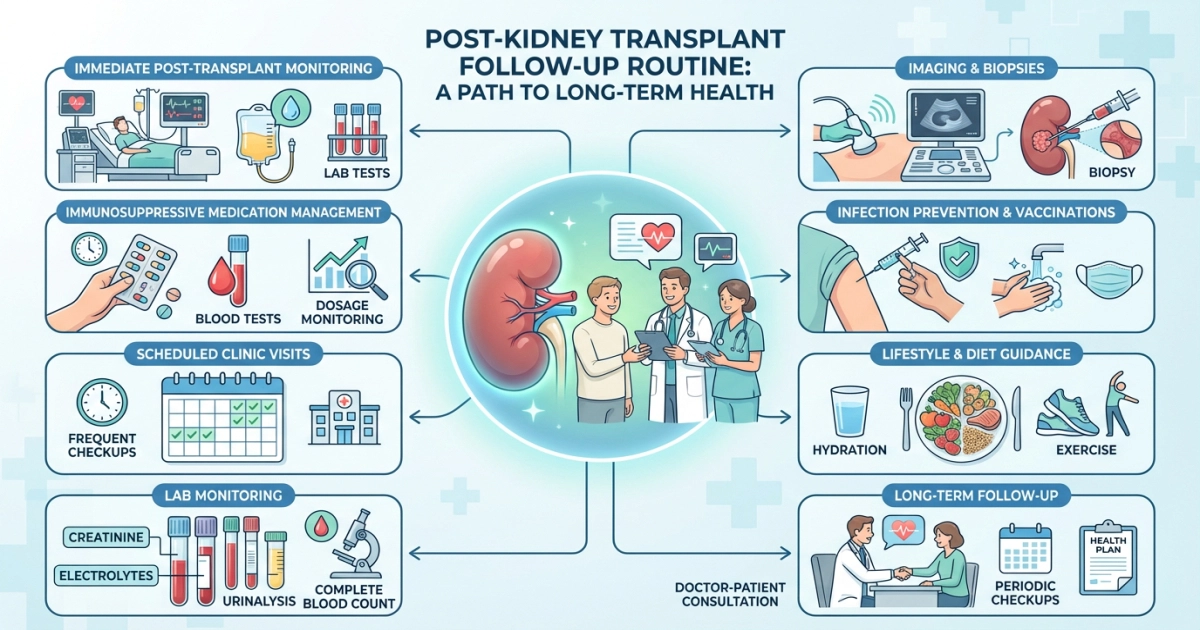
Life after a kidney transplant depends heavily on disciplined follow-up care. This includes regular clinic visits, lifelong immunosuppressive medication, routine lab monitoring, and informed lifestyle changes. With proper follow-up, one-year graft survival now exceeds 95% in many centers. The keys to long-term success include medication adherence, early detection of complications, heart-healthy habits, and strong mental support systems.
Immediate Post-Op Recovery: Building a Stable Foundation
The first few weeks after surgery are critical for protecting your transplanted kidney.
Most patients remain in the hospital for 3–5 days for close monitoring of urine output, fluid balance, and early graft function. Urine production is checked frequently, and increasing output is usually an encouraging sign that the new kidney is working.
Wound care, mobility, and hydration are essential during this phase. Clean the incision as instructed, avoid heavy lifting, and gradually increase activity through short walks. Many centers recommend avoiding driving for at least two weeks.
Fatigue is common. Instead of forcing activity, take structured rest periods and increase your workload slowly. Pushing too hard early on increases the chance of complications or readmission.
Hydration is important. Most recipients are advised to drink 2–3 liters of water per day unless otherwise directed by their transplant team.
Medication Management: Preventing Organ Rejection
Immunosuppressive medications are lifelong and non-negotiable.
Most patients take:
- Tacrolimus or Cyclosporine
- Mycophenolate
- Prednisone (often tapered)
Missing doses is one of the leading causes of transplant rejection. Pill organizers, phone alarms, or medication apps can significantly reduce missed doses.
Extended-release immunosuppressants are becoming more common in 2025, helping some patients move to once-daily dosing and simplifying adherence.
Regular blood tests are required to monitor drug levels. For tacrolimus, levels are generally maintained in the range of 5–10 ng/mL, depending on the stage and your doctor’s plan.
Always consult your pharmacist or transplant team before taking over-the-counter drugs or supplements, as many can interfere with immunosuppressants.
Regular Check-Ups and Monitoring
Follow-up schedules are structured but may vary by center:
- Weeks 1–4: Weekly visits
- Month 2–3: Every two weeks
- Month 4–12: Monthly
- After year one: Every 3–6 months
These visits track:
- Creatinine levels
- Electrolytes
- Blood pressure
- Drug levels
- Signs of infection or rejection
Home blood pressure monitoring is strongly recommended. Aim for readings below 130/80 mmHg, unless your doctor advises otherwise.
In 2025, some centers integrate AI-assisted monitoring tools and telehealth systems to help track trends and identify risks earlier.
Lifestyle Adjustments: Supporting Long-Term Kidney Health
After transplantation, lifestyle choices directly impact graft survival.
Diet tips:
- Limit sodium intake to under 2g daily
- Eat lean proteins and plenty of vegetables
- Avoid undercooked or raw foods due to infection risk
- Stay well hydrated
Exercise guidelines:
- Start slowly with walking
- Aim for 150 minutes/week of moderate activity
- Include light strength training after recovery approval
Weight control, blood sugar monitoring, and cholesterol management are also essential since transplant medications increase the risk of diabetes and cardiovascular disease.
Recognizing and Preventing Rejection
Rejection can be subtle. Common warning signs include:
- Fever
- Reduced urine output
- Swelling
- Increased fatigue
- Pain over the transplant area
- Sudden rise in blood pressure
Routine blood work often detects rejection before symptoms appear. Never ignore unusual changes — early treatment significantly improves outcomes.
Emotional and Psychological Support
Mental health plays a major role in recovery and long-term success.
Many transplant recipients experience:
- Anxiety
- Depression
- Fear of rejection
- Guilt toward donors
Support groups, therapy, and transplant counseling programs can help reduce this psychological burden. Staying socially connected and communicating with family and friends also improves adjustment and long-term adherence.
Long-Term Health Maintenance
After the first year, follow-ups may reduce in frequency, but ongoing care is still crucial.
Key long-term priorities include:
- Annual cancer screenings
- Bone health monitoring
- Regular vaccinations (avoid live vaccines unless approved)
- Skin protection due to higher skin cancer risk from immunosuppression
Daily sunscreen use (SPF 50 or higher) is strongly advised for all transplant patients.
Travel and Daily Life After Transplant
Most patients can resume travel after 3 months, once stable.
Travel tips:
- Carry extra medications (double supply)
- Keep prescriptions and doctor’s letters
- Identify nearby medical centers before trips
- Maintain your monitoring routine
Normal activities, work, exercise, travel, and personal relationships can usually resume with medical guidance.
Innovations in 2025 Transplant Follow-Up Care
Current advancements include:
- AI-driven rejection risk prediction tools
- Smart medication tracking apps
- Integration of wearable health monitoring devices
- Hybrid telehealth and in-person care models
These technologies improve early detection and personalize follow-up plans, but they complement not replace routine medical care.
People Also Ask
- How often do I need blood tests after a kidney transplant?
- What foods should I avoid post-transplant?
- When can I start exercising after kidney transplant?
- What are the early signs of transplant rejection?
- How long does a transplanted kidney last?
- Is traveling safe after a kidney transplant?
- What new treatments are available for kidney transplant patients in 2025?
Author Bio:
Dr. ADAM is a nephrology specialist with over 15 years of experience in transplant medicine, having supported hundreds of kidney transplant patients through recovery and long-term care. He focuses on practical patient education and evidence-based follow-up strategies.
Disclaimer: This article provides general information based on medical guidelines and patient experiences. Always consult your transplant team for personalized medical advice. This content does not replace professional care.