Do Kidney Stones Cause Diarrhea?
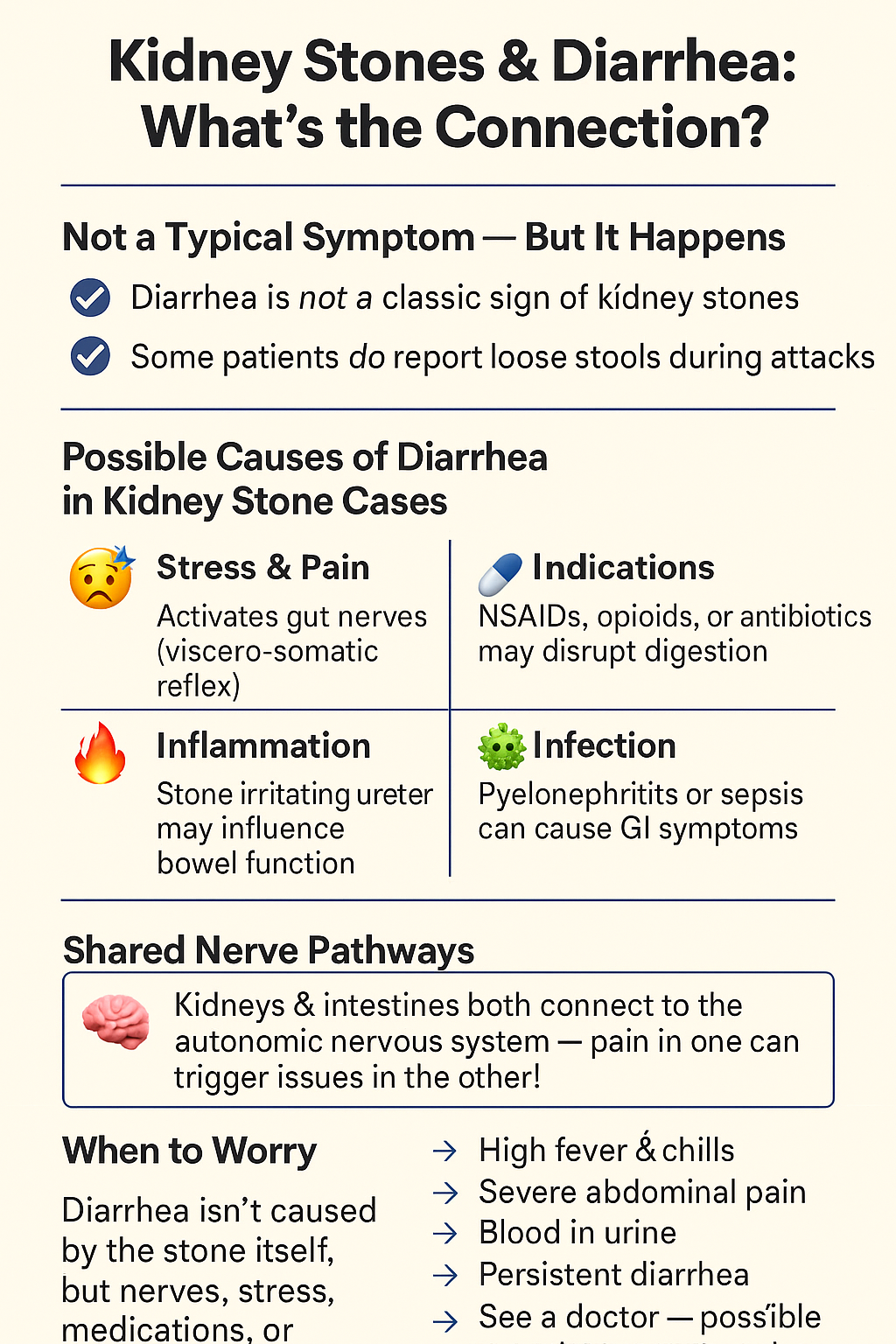
Yes, diarrhea can happen in people with kidney stones, but not directly due to the stone. It’s usually a secondary symptom of pain, stress, medications, or complications from the stone or its treatment.
Is Diarrhea a Symptom of Kidney Stones?
Why It’s Rarely Noted But Why It Can Still Occur in Some Situations
Diarrhea isn’t considered a classic symptom of kidney stones. Typically, symptoms include:
- Sharp, cramping pain in the back and side.
- Blood in the urine
- Frequent urination
- Nausea and vomiting
However, some patients report loose stools or an urgent need to defecate during a kidney stone attack. While it’s not directly caused by the stone itself, it can occur due to a few key physiological mechanisms.
The Role of Referred Pain and Autonomic Nerve Disruption
The kidneys and intestines connect through the spinal cord and autonomic nervous system. Pain from a kidney stone can cause a “spillover” effect. This activates nerves that affect bowel motility. This phenomenon is known as visceral cross-talk. It can confuse the body’s response and lead to bowel changes, such as diarrhea.
What Is the Connection Between Kidney Stones and Diarrhea?
Indirect Mechanisms: Pain, Stress Response, and Ureter Irritation
When a stone irritates the ureter, it can cause severe inflammation. This stress activates the sympathetic nervous system. It can also affect gut motility and digestion. For some people, this leads to cramping or diarrhea.
Interaction With Medications Like Opioids or NSAIDs
Pain management is important. NSAIDs can upset the stomach. Opioids may slow digestion but can cause rebound diarrhea during withdrawal or dose changes. Even antibiotics for infections can disrupt the gut microbiome, leading to diarrhea.
Can Kidney Stones Trigger IBS-like Symptoms?
Overlap With Irritable Bowel Syndrome
Many patients with kidney stones report IBS-like symptoms during acute episodes — even if they don’t have a formal diagnosis. Why?
- Both conditions involve the viscero-somatic reflexes (gut and nerve signaling).
- Stress and pain from stones can exacerbate gut sensitivity.
- Dehydration or dietary triggers may affect both kidneys and the bowel.
How Some Patients Report GI Symptoms Alongside Stones
Some patients report “gut-wrenching” pain along with urgency or diarrhea during a stone episode. These symptoms are often confused with food poisoning or a GI infection. They usually go away once the stone passes.
Medical Situations Where Both Occur Together
When Stones Cause Infection (e.g., Pyelonephritis) or Sepsis
Infections like pyelonephritis (a kidney infection) can cause systemic symptoms, including:
- Fever and chills
- Nausea, vomiting
- Diarrhea
In serious cases like urosepsis, diarrhea may be a systemic inflammatory response.
Secondary Symptoms From Severe Obstruction or Inflammation
A completely blocked ureter can cause hydronephrosis, inflammation, and even affect abdominal organs — indirectly leading to bowel irregularity or diarrhea.
What Are the Gastrointestinal Symptoms Associated With Kidney Stones?
Nausea and Vomiting
This is one of the most common GI symptoms in kidney stone patients. The intense pain can stimulate the vomiting center in the brain. Additionally, obstruction or infection may lead to gastric irritation.
Bloating and Abdominal Pain
Pain radiating from the kidney can feel like it’s coming from the stomach or lower abdomen — especially in the case of lower ureteric stones. This often leads to misdiagnoses like:
- Gastritis
- Appendicitis
- Diverticulitis
Diarrhea and Bowel Irregularity
Stress, inflammation, and nerve signaling can all trigger bowel changes. Even if diarrhea isn’t directly caused by the stone, it may be a reaction to pain, medication, or dehydration.
Constipation From Medications
Pain medications (especially opioids) are well known to slow gut motility. Constipation can increase abdominal pressure, making it difficult to differentiate from kidney-related discomfort.
What Are the Causes of Kidney Stones?
What Leads to the Formation of Kidney Stones?
Stones form when your urine contains too much crystal-forming substances like calcium, oxalate, or uric acid — and not enough fluid to dilute them. Risk factors include:
- Dehydration
- Obesity
- High-protein or high-sodium diets
- Genetics
- Gut absorption issues
What Types of Kidney Stones Can Form?
- Calcium Oxalate: Most common; linked to oxalate-rich foods and low calcium intake
- Uric Acid: More common in those with gout or high-purine diets
- Struvite: Associated with chronic urinary infections
- Cystine: Rare, genetic
Relation of Each to GI Factors
Some stones are tied to malabsorption syndromes (e.g., Crohn’s disease, gastric bypass), where excess fat binds calcium, allowing more oxalate to be absorbed — leading to calcium oxalate stones.
How Do Kidney Stones Affect Bowel Movements?
Shared Nerve Pathways (Visceral Cross-Talk)
Nerves from the T10–L2 spinal segments serve both the kidneys and parts of the bowel. So, kidney pain can stimulate bowel activity — and vice versa — leading to unexpected GI symptoms during stone episodes.
Can Stones Lead to Diarrhea Through Dehydration?
Yes. Dehydration is a double threat:
- It concentrates urine, increasing stone risk
- It also impairs digestion and can lead to diarrhea or constipation
Impact of Pain Meds and Antibiotics
- Opioids: Cause constipation → rebound diarrhea in some cases
- NSAIDs: May irritate the GI lining
- Antibiotics: Often cause antibiotic-associated diarrhea, especially if gut flora is disrupted
How to Prevent Kidney Stones (and Possibly Related GI Symptoms)
What Lifestyle Changes Help?
- Exercise supports kidney function and improves gut motility
- Stress reduction can prevent both kidney and bowel flare-ups
- Routine hydration checks (pale urine = well hydrated)
What Dietary Choices Reduce Stone Risk?
- Limit oxalate (e.g., spinach, nuts, chocolate)
- Pair oxalate foods with calcium to prevent absorption
- Moderate animal protein and salt
- Avoid food triggers that irritate your gut (spicy foods, caffeine, high-FODMAPs)
How Important Is Hydration in Prevention?
Extremely. Aim for 2.5–3 liters of fluid daily unless your doctor says otherwise. Hydration:
- Dilutes urine (reducing stone risk)
- Supports regular bowel movements
- Helps prevent dehydration-related diarrhea
Tip: Add cucumber slices or citrus to water for better taste and mild diuretic benefits.
Real Case Examples & Research Insights
Case Study: 45-Year-Old With GI Symptoms and Stones
A man presented to the ER with cramping, diarrhea, and lower abdominal pain. Initially diagnosed with a GI bug, imaging later showed a 5mm stone lodged in the ureter. After passing the stone, his symptoms resolved completely.
Research: GI Disorders and Stone Formation
As per a research published in the Journal of Urology, individuals with inflammatory bowel disease (IBD) and those who have had bariatric surgery are considerably more prone to develop kidney stones especially calcium oxalate.
“The gut-kidney axis is real. What affects one often affects the other,” says Dr. Lisa Kim, nephrologist at the Cleveland Clinic.
Patient Experience
“I thought I had food poisoning. I had stomach cramps, loose stools, and nausea — then out of nowhere, this stabbing pain hit my side. Turned out it was a kidney stone,” said Sarah, 38, from Austin, TX.
Frequently Asked Questions (FAQs)
Yes depending on pain level, medications, and hydration status, you might alternate between the two.
Yes. Referred pain and ureter inflammation can mimic abdominal cramps.
If symptoms last more than 48 hours, or you have fever, vomiting, or blood in urine/stool, seek medical attention.
Yes. Some antibiotics can disrupt gut flora and lead to temporary diarrhea.
Yes it can cause dehydration, which increases the risk of stone formation or worsening.
Must Read These Interesting Articles
- 7-Day Kidney Stone Diet Chart for Natural Relief
- Occult Blood in Urine: What It Means and When to Worry
- Low Potassium Diet for Kidney Health
Sources & Expert References
- Mayo Clinic
- Cleveland Clinic
- National Kidney Foundation
- Journal of Urology: GI Symptoms in Stone Patients
- NIH: “Kidney Stones and Gastrointestinal Disease”
Final Thought: The Gut-Kidney Connection
Kidney stones can surprisingly affect your gut, especially during an acute episode. Knowing how your kidneys and digestive system interact helps you spot symptoms early. This knowledge can improve your health management.
💡 Myth Buster: Kidney stones don’t always cause urinary pain first — for some, the first signs show up in the gut.