Introduction: When Two Troubles Collide
Picture this: You’re just getting over the pain of passing a kidney stone, and bam! You’re hit with that annoying, burning feeling of a bladder infection. Are they linked? As a urologist with more than 15 years under my belt, I’ve seen tons of patients deal with this annoying overlap. Kidney stones and bladder infections (UTIs) are different issues, but they can totally mess with each other in a nasty cycle. This guide is here to clear things up, showing you how kidney stones can lead to UTIs, all backed by solid evidence and some handy tips to keep your urinary health in check. Let’s jump in!
Understanding Kidney Stones: More Than Just Pain
What Exactly Are Kidney Stones?
Kidney stones are hardened mineral deposits that form when your urine becomes oversaturated. Think of them like unwanted crystals growing in your kidneys when substances like calcium, oxalate, or uric acid can’t stay dissolved, leading to type of kidney stones. Dehydration is often the biggest culprit, concentrating these minerals until they clump together.
The Four Main Culprits: Stone Types Explained
- Calcium Oxalate Stones (Most Common – 80%):
- Cause: Certain medical conditions can increase the likelihood of developing kidney stones. High oxalate intake (spinach, nuts, chocolate) combined with low urine volume or calcium imbalance may increase the risk of forming stones.
- Prevention Tip: Pair high-oxalate foods with calcium-rich sources (e.g., spinach salad with cheese). This binds oxalate in the gut, preventing absorption.
- Uric Acid Stones (5-10%):
- Cause: Chronically acidic urine (pH <5.5) often linked to high purine diets (red meat, shellfish), gout, or metabolic syndrome.
- Prevention Tip: Alkalinize urine with lemon water or potassium citrate supplements. Limit animal proteins.
- Struvite Stones (10-15%):
- Cause: Directly linked to UTIs. Bacteria like Proteus mirabilis break down urea into ammonia, creating an alkaline urine environment perfect for these fast-growing type of kidney stones.
- Risk: Can form “staghorn” calculi filling the kidney, risking permanent damage.
- Cystine Stones (Rare – <1%):
- Cause: Genetic disorder (cystinuria) causing excessive cystine leakage into urine.
- Management: Focus on preventing kidney stones through dietary changes and hydration. Requires aggressive hydration and specialized medications (e.g., tiopronin).
Beyond the Classic “Colic”: Recognizing Stone Symptoms
While sudden, excruciating flank pain (renal colic) is classic, stones can also cause persistent discomfort in the ureter and kidney.
- Persistent lower abdominal or groin aches.
- Blood in urine (hematuria) – often microscopic, only visible under a microscope, can be a symptom of kidney stones.
- Urinary urgency or frequency, mimicking a UTI.
- Nausea/vomiting due to shared nerve pathways with the gut.
Bladder Infections (UTIs): The Unwanted Intruders
How UTIs Take Hold
A bladder infection occurs when bacteria (usually E. coli from the gut) ascend the urethra and multiply in the bladder. While uncomfortable, an uncomplicated UTI is usually confined to the bladder. The real danger arises if it spreads upwards to the kidneys, potentially causing more severe symptoms of kidney stones.pyelonephritis), especially if a stone is blocking the path.
Why Women Bear the Brunt (and What Men Should Know)
Women are disproportionately affected due to anatomy:
- A significantly shorter urethra gives bacteria easier access to the urinary tract.
- Proximity of the urethral opening to the anus.
- Hormonal shifts (pregnancy, menopause) altering urinary defenses.
Men, take note: While less common, UTIs in men are often considered “complicated” from the start and frequently signal an underlying issue like an obstructing stone or enlarged prostate.
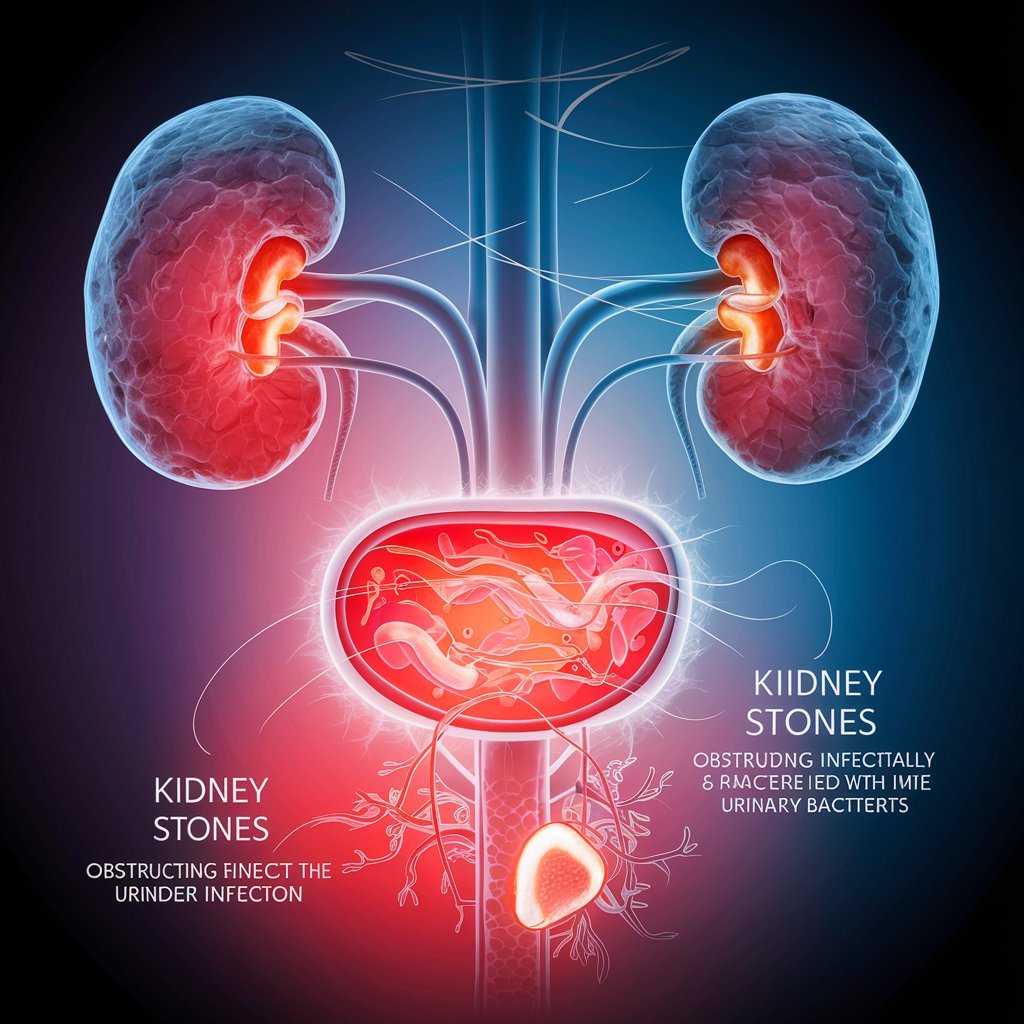
The Critical Link: How Kidney Stones Can Cause Bladder Infections
Kidney stones don’t directly cause pain. create bacteria, but they create the perfect storm for UTIs to flourish through three key mechanisms:
- Urinary Obstruction & Stagnant Pools:
- The Process: A stone blocking the ureter (tube from kidney to bladder) or urethra halts urine flow. Stagnant urine in the bladder is like a stagnant pond – a breeding ground for bacteria.
- Evidence: A pivotal 2022 study in urology BJU International found that 35% of patients with obstructing stones developed UTIs within just 48 hours. Removing the stone promptly reduced infection rates by 70%.
- Patient Story: I recall a patient, Sarah, whose recurrent UTIs only resolved after we discovered and removed a small, obstructing stone near her ureterovesical junction – a hidden culprit missed on initial ultrasounds.
- Mucosal Damage: Opening the Gates:
- The Process: Sharp-edged stones (like calcium oxalate) scrape and irritate the delicate lining of the ureters and bladder as they pass. This creates microscopic tears and inflammation, making it easier for bacteria to latch on and invade the tissue.
- Prevention Focus: Understanding the common type of kidney stone can aid in prevention efforts. Staying hyper-hydrated during stone passage isn’t just about flushing the stone; it dilutes irritants and reduces friction on damaged tissues.
- The Struvite Stone-Infection Cycle (A Self-Feeding Loop) can lead to severe urinary tract infections.
- Step 1: A UTI starts, caused by urease-producing bacteria (Proteus, Klebsiella, some Staph).
- Step 2: Identify the type of stone to tailor prevention strategies. These bacteria split urea into ammonia, drastically raising urine pH (making it alkaline).
- Step 3: This alkaline environment is ideal for struvite (and sometimes calcium phosphate) stones to form rapidly.
- Step 4: The stone itself becomes a biofilm-coated “fortress,” harboring bacteria and shielding them from antibiotics, perpetuating the infection.
- Treatment Imperative: Breaking this cycle requires a dual attack: targeted antibiotics AND complete surgical removal of the stone (via PCNL or ureteroscopy). Leaving fragments behind almost guarantees recurrence.
The Bidirectional Relationship: UTIs Can Fuel Stones Too
It’s not a one-way street. Chronic or recurrent UTIs, especially with urease-producing bacteria, are a primary cause of struvite stones. Inflammation from persistent infection can also alter urine chemistry, potentially promoting other stone types.
Protecting Yourself: Preventing UTIs When You Have Kidney Stones
Your Proactive Defense Plan
- Hydration: Non-Negotiable Foundation
- Goal: 2.5-3 liters of water daily (more if sweating). Your urine should be pale yellow/clear.
- Why it Works: Dilutes stone-forming minerals and flushes bacteria out before they can colonize.
- Expert Tip: Stay hydrated to help prevent urinary tract infections. Add fresh lemon juice! Citrate binds calcium and inhibits stone growth while acidifying urine (helpful for calcium stones and UTIs).
- Dietary Modifications: Strategic Eating to prevent kidney stones may be beneficial.
- For Calcium Oxalate Stones: Reduce high-oxalate foods (spinach, beets, nuts, chocolate), but don’t cut calcium. Pair high-oxalate foods with calcium sources (e.g., almonds with yogurt).
- For Uric Acid Stones: Limit purines (red meat, organ meats, shellfish, beer). Emphasize fruits/veggies to alkalinize urine.
- Universal: Drastically reduce sodium (<2300mg/day) to lower urinary calcium. Minimize added sugars (promotes bacterial growth).
- Hygiene & Habits: Daily Defense
- Urinate Frequently: Don’t hold it! It may cause the kidney to stop working. Empty your bladder every 3-4 hours and always after sex.
- Wipe Front-to-Back: Essential for women to prevent gut bacteria spread.
- Choose Breathable Fabrics: Cotton underwear reduces moisture where bacteria thrive.
- Consider Probiotics: Certain strains like those causing urinary tract infections can contribute to kidney stone formation. Lactobacillus rhamnosus GR-1 and L. reuteri RC-14 (oral or vaginal) can help maintain healthy vaginal flora, a key defense against UTIs in women.
- Medical Prophylaxis: When Lifestyle Isn’t Enough
- Potassium Citrate: Prescribed to alkalinize urine (dissolves uric acid stones) and increase protective citrate levels.
- Low-Dose Antibiotics: For patients with recurrent UTIs linked to stones, a nightly low dose (e.g., Nitrofurantoin 50mg or Trimethoprim) for 3-6 months can be highly effective as a bridge while addressing the stone issue.
- Methenamine Hippurate: A non-antibiotic urinary antiseptic converting to formaldehyde in acidic urine, useful for some patients with recurrent infections.
Diagnosis & Treatment: Navigating Both Conditions
Getting the Right Diagnosis
- Kidney Stones: Non-contrast CT scan is the gold standard. Ultrasound is good for monitoring and in pregnancy/children. A 24-hour urine test reveals underlying metabolic abnormalities driving stone formation.
- UTIs: Urinalysis (looks for white blood cells, nitrites) and Urine Culture & Sensitivity (identifies the exact bacteria and best antibiotics) are crucial. Always request a culture if you have stones and a suspected UTI.
Treatment Tailored to the Problem
- Small Stones (<5mm): “Watchful waiting” with hydration, pain control (NSAIDs like ibuprofen), and potentially an alpha-blocker (Tamsulosin) to relax the ureter.
- Large or problematic stones in the urinary system may cause significant pain and require imaging tests.
- Shock Wave Lithotripsy (SWL): Breaks stones externally with sound waves.
- Ureteroscopy (URS): A scope passed up the urethra/bladder/ureter to laser and remove stones. Often best for stones linked to UTIs as it allows direct access to the ureter and kidney for clearing of fragments.
- Percutaneous Nephrolithotomy (PCNL): Surgery for very large or complex stones (like staghorns), involving a small back incision.
- Treating UTIs in Stone Formers:
- Uncomplicated UTI: A short course (3 days) of Nitrofurantoin or Fosfomycin is often sufficient.
- Complicated UTI (or with stones): Requires a longer course (7-14 days) of a broader-spectrum antibiotic (e.g., Ciprofloxacin, Levofloxacin, Ceftriaxone) based on culture results. Crucially, if an obstructing stone is present, relieving the blockage (with a stent or nephrostomy tube) is often necessary alongside antibiotics for the infection to clear.
Red Flags: When to Seek Emergency Care
Don’t wait! Seek immediate medical attention if you experience:
- Fever above 101°F (38.3°C) with chills or flank pain (sign of kidney infection/pyelonephritis).
- Inability to urinate (anuria) or only passing a few drops despite intense urgency (suggests complete obstruction).
- Severe, unrelenting pain or vomiting may prevent fluid intake, potentially leading to kidney stones.
- Confusion, dizziness, or rapid heartbeat (potential signs of sepsis, a life-threatening response to infection).
Timely intervention is critical to prevent kidney damage, sepsis, or other serious complications.
Conclusion: Breaking the Cycle, Taking Control
The link between kidney stones and bladder infections is undeniable and often bidirectional. Stones create physical blockages, cause tissue damage, and can even form biofilms that harbor bacteria, significantly increasing UTI risk. Conversely, certain UTIs directly cause struvite stones. The key to breaking this cycle lies in proactive management: relentless hydration, targeted dietary changes, meticulous hygiene, and prompt medical evaluation for both stones and infections. If you’re a stone former experiencing recurrent UTIs, consult a urologist. A comprehensive evaluation, including imaging and metabolic testing, can identify the specific link and tailor a prevention strategy to safeguard your long-term urinary health. You don’t have to live in a loop of pain and infection.
Frequently Asked Questions (FAQs)
No, UTIs do not dissolve stones. In fact, they often complicate stone treatment. Struvite stones require surgical removal alongside antibiotics to eradicate the infection fully.
Clues include a history of stones, concurrent severe flank or abdominal pain (especially colicky pain), visible blood in the urine (gross hematuria), or a UTI that doesn’t resolve with standard antibiotics. Imaging (CT scan) is definitive.
Yes. Repeated infections, especially alongside stones, increase risks of kidney scarring (chronic pyelonephritis), high blood pressure, decreased kidney function, and in severe cases, kidney failure. It also promotes struvite stone growth.
Proceed with caution! Cranberry may help prevent some UTIs by preventing bacteria from sticking to the bladder wall. However, it’s high in oxalates. If you form calcium oxalate stones, cranberry juice/supplements might increase your stone risk. Discuss alternatives (like D-Mannose) with your doctor.
Indirectly, yes. Chronic stress can weaken the immune system, potentially making you more susceptible to infections that may cause kidney stones. It can also lead to dehydration (forgetting to drink water) or poor dietary choices (high salt, sugar), both of which promote stone formation. Prioritizing stress management is part of holistic urinary health.
Some irritation and minor infection risk exist temporarily after procedures like ureteroscopy (due to the stent). However, recurrent UTIs post-procedure warrant investigation. It could indicate residual stone fragments harboring bacteria, an untreated metabolic issue, or another anatomical problem. Bring this up persistently with your urologist.

