Asthma is a chronic respiratory condition that affects millions worldwide, yet misconceptions and incomplete knowledge persist. To truly grasp what is asthma, we must delve beyond surface definitions and explore its complex nature, triggers, and management strategies. This article offers a deeply researched, nuanced perspective designed to empower readers with expert insights, practical wisdom, and actionable advice for living well with asthma.
Defining Asthma: More Than Just Wheezing
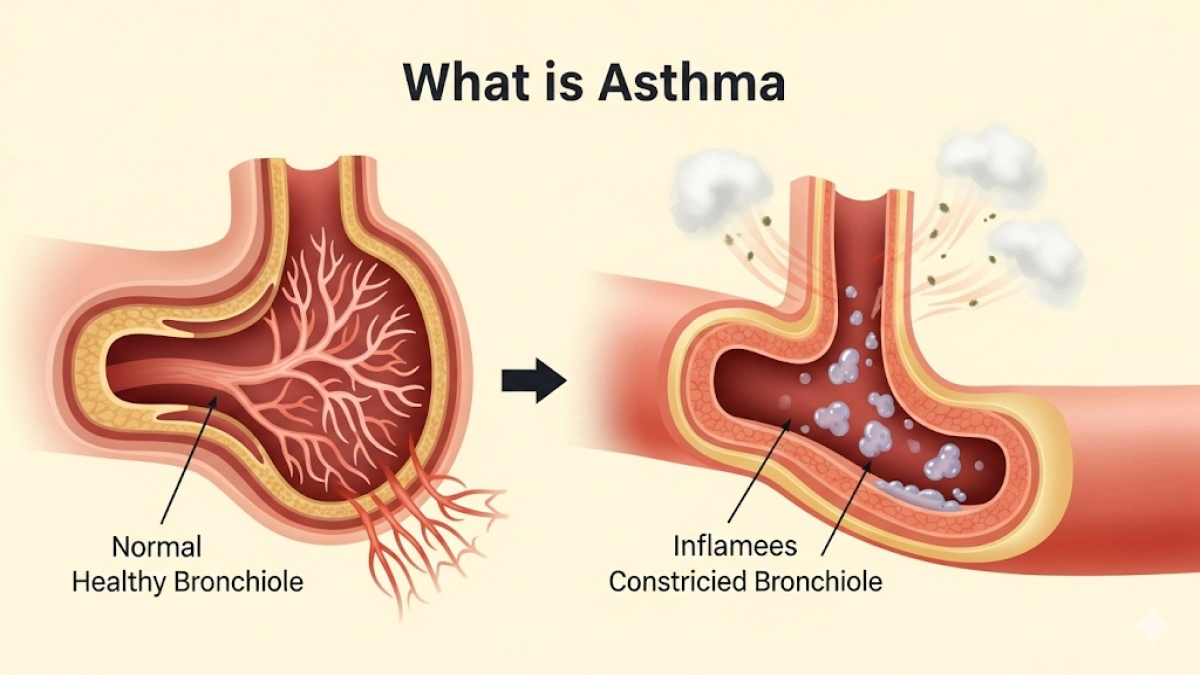
At its core, asthma is a chronic inflammatory disease of the airways characterized by episodes of airflow obstruction and bronchial hyperresponsiveness. This means the bronchial tubes—air passages in the lungs—become inflamed and narrowed, making breathing difficult. Unlike a one-time respiratory infection, asthma is a persistent condition with variable symptoms that can flare unpredictably.
Key Features of Asthma
- Airway Inflammation: Persistent swelling and irritation inside the bronchial tubes.
- Bronchoconstriction: Tightening of the muscles around airways during attacks.
- Excess Mucus Production: Further blocks airflow.
- Variable Symptoms: Wheezing, coughing, chest tightness, and shortness of breath.
Understanding these mechanisms is crucial because asthma is not a uniform disease; it manifests differently across individuals, influenced by genetics, environment, and lifestyle.
The Science Behind Asthma: Pathophysiology Explained
Asthma’s complexity lies in its multifactorial pathophysiology. The immune system plays a pivotal role, often overreacting to harmless substances (allergens) or irritants, triggering a cascade of inflammatory responses.
Immune Response and Inflammation
When exposed to triggers such as pollen, dust mites, or smoke, the immune system releases inflammatory mediators like histamines and leukotrienes. These chemicals cause:
- Swelling of airway linings.
- Increased mucus secretion.
- Constriction of smooth muscles around airways.
This triad leads to the hallmark symptoms of asthma attacks.
Chronic vs. Acute Phases
- Chronic Phase: Ongoing inflammation even without symptoms, leading to airway remodeling (structural changes).
- Acute Exacerbations: Sudden worsening of symptoms requiring immediate intervention.
Causes and Triggers: What Sparks Asthma?
Asthma’s origins are a blend of genetic predisposition and environmental exposures. Identifying and managing triggers is a cornerstone of effective asthma control.
Common Triggers Include:
- Allergens: Pollen, pet dander, mold, dust mites.
- Irritants: Tobacco smoke, air pollution, strong odors.
- Respiratory Infections: Colds, flu, sinus infections.
- Physical Activity: Exercise-induced bronchoconstriction.
- Weather Changes: Cold air or sudden temperature shifts.
- Stress and Emotions: Psychological factors can exacerbate symptoms.
Symptoms: Recognizing Asthma Early
Asthma symptoms can be subtle or severe, often fluctuating over time. Early recognition is vital to prevent complications.
Typical Symptoms:
- Wheezing (a whistling sound when breathing out).
- Persistent coughing, especially at night or early morning.
- Shortness of breath or rapid breathing.
- Chest tightness or pain.
When to Seek Medical Help
- Difficulty speaking or walking due to breathlessness.
- Blue lips or fingernails (signs of low oxygen).
- Symptoms not relieved by prescribed inhalers.
Diagnosing Asthma: Tests and Evaluations
Accurate diagnosis requires a combination of clinical history, physical examination, and objective testing.
Diagnostic Tools:
- Spirometry: Measures lung function and airflow obstruction.
- Peak Flow Monitoring: Tracks breathing capacity over time.
- Allergy Testing: Identifies specific allergens.
- Exhaled Nitric Oxide Test: Assesses airway inflammation.
Treatment and Management: Beyond the Inhaler
Asthma management is a dynamic process tailored to individual needs, aiming to minimize symptoms and prevent attacks.
Pharmacological Treatments
- Reliever Inhalers (Short-Acting Beta-Agonists): Provide quick symptom relief.
- Controller Medications (Inhaled Corticosteroids): Reduce inflammation long-term.
- Leukotriene Modifiers: Target inflammatory pathways.
- Biologics: Advanced therapies for severe asthma targeting specific immune components.
Lifestyle and Environmental Control
- Avoid known triggers.
- Maintain a clean, allergen-free home environment.
- Use air purifiers and humidity control.
- Regular exercise with proper warm-up.
- Stress management techniques.
Action Plan Development
Patients should work with healthcare providers to create personalized asthma action plans, detailing daily management and steps during exacerbations.
Living with Asthma: Practical Wisdom and Quality of Life
Asthma need not limit life’s possibilities. With informed management, individuals can lead active, fulfilling lives.
Tips for Daily Living
- Monitor symptoms and peak flow regularly.
- Communicate openly with healthcare providers.
- Educate family and friends about asthma.
- Prepare for emergencies with accessible inhalers.
- Stay updated on vaccinations to prevent respiratory infections.
Emerging Research and Future Directions
The landscape of asthma care is evolving rapidly, with promising research into genetic markers, novel biologics, and digital health tools for monitoring.
Innovations to Watch
- Precision medicine approaches tailoring treatment to genetic profiles.
- Smart inhalers with adherence tracking.
- AI-driven predictive models for asthma attacks.
Conclusion: Asthma Is Manageable with Knowledge and Care
Understanding what is asthma in its full complexity empowers patients, caregivers, and clinicians alike. This chronic condition, while challenging, can be effectively controlled through a combination of medical treatment, lifestyle adjustments, and ongoing education. By embracing a holistic approach grounded in expertise and trustworthiness, individuals with asthma can breathe easier and live better.