Anal fissures, though often a sensitive and private topic, affect a significant portion of the population at some point in their lives. These small tears in the lining of the anal canal can cause intense discomfort, pain, and bleeding, impacting quality of life. Despite their prevalence, misconceptions and stigma often prevent open discussion and timely treatment. This article aims to provide a comprehensive, expert-informed exploration of the causes and treatments of anal fissures, blending clinical knowledge with practical advice to empower readers toward effective healing and prevention.
What Is an Anal Fissure?
An anal fissure is a small tear or crack in the mucosal lining of the anus. This delicate tissue can become damaged due to various factors, leading to pain during bowel movements, bleeding, and sometimes itching or irritation. While the fissure itself is typically minor, the symptoms can be disproportionately severe, often causing a cycle of pain and muscle spasm that hinders healing.
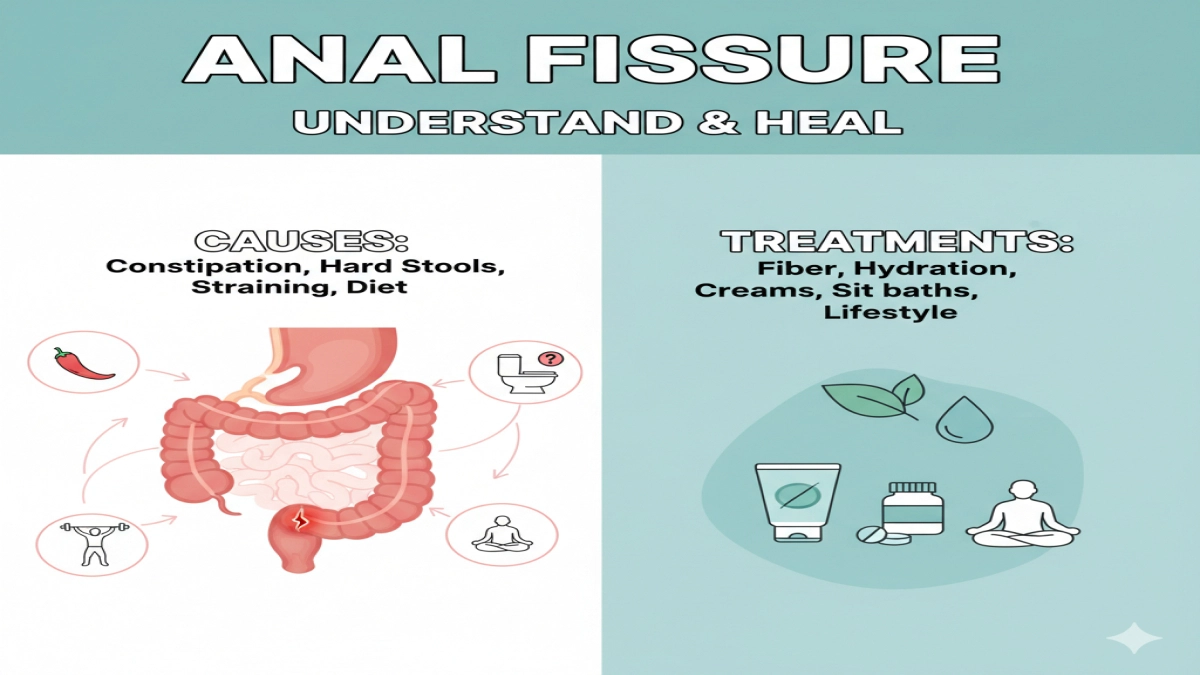
Causes of Anal Fissures: A Closer Look
Understanding the root causes is essential for effective treatment and prevention. The development of an anal fissure usually involves a combination of mechanical trauma and physiological factors.
1. Mechanical Trauma
- Constipation and Hard Stools: The most common cause is the passage of hard or large stools that stretch and tear the anal lining. Chronic constipation exacerbates this risk.
- Straining During Bowel Movements: Excessive straining increases pressure on the anal canal, making the tissue more susceptible to injury.
- Diarrhea: Frequent loose stools can irritate and inflame the anal mucosa, increasing vulnerability to fissures.
- Childbirth: Vaginal delivery can sometimes cause fissures due to the strain and pressure on the pelvic floor and anal region.
2. Physiological and Medical Factors
- Anal Sphincter Spasm: A key factor in fissure formation and persistence is the involuntary spasm of the internal anal sphincter muscle. This spasm reduces blood flow to the area, impairing healing.
- Inflammatory Conditions: Diseases such as Crohn’s disease or other inflammatory bowel diseases can cause fissures due to chronic inflammation.
- Infections: Certain infections, including sexually transmitted infections, can contribute to fissure development.
- Poor Blood Supply: Reduced circulation in the anal region, sometimes due to age or vascular conditions, can delay healing.
3. Lifestyle and Dietary Influences
- Low Fiber Intake: Diets lacking sufficient fiber lead to harder stools and constipation.
- Dehydration: Insufficient fluid intake thickens stool consistency.
- Sedentary Lifestyle: Reduced physical activity can slow bowel motility, increasing constipation risk.
Recognizing Symptoms: When to Seek Help
Anal fissures typically present with a distinct set of symptoms:
- Sharp, burning pain during and after bowel movements
- Bright red blood on toilet paper or stool surface
- Itching or irritation around the anus
- Visible crack or tear in the anal skin (in some cases)
- Muscle spasms causing discomfort
If symptoms persist beyond a few weeks or worsen, it is crucial to consult a healthcare professional to rule out other conditions and receive appropriate care.
Treatment Strategies: From Home Care to Medical Intervention
Treatment aims to relieve pain, promote healing, and prevent recurrence. Approaches vary depending on the fissure’s severity and chronicity.
1. Conservative Home Remedies
- Dietary Adjustments: Increasing fiber intake through fruits, vegetables, and whole grains softens stools, reducing trauma during defecation.
- Hydration: Drinking ample water daily helps maintain stool softness.
- Sitz Baths: Warm water baths for 10-15 minutes several times a day relax the anal sphincter and improve blood flow.
- Topical Emollients: Applying barrier creams or petroleum jelly can protect the fissure from irritation.
- Avoid Straining: Adopting proper bowel habits and avoiding prolonged sitting on the toilet can reduce pressure.
2. Medical Treatments
- Topical Nitroglycerin: This medication relaxes the anal sphincter muscle, improving blood flow and promoting healing. It may cause headaches as a side effect.
- Calcium Channel Blockers: Topical agents like diltiazem or nifedipine serve a similar purpose with fewer side effects.
- Botulinum Toxin (Botox) Injections: Botox temporarily paralyzes the sphincter muscle, reducing spasm and allowing healing.
- Pain Relief: Over-the-counter analgesics or prescribed medications can manage discomfort.
3. Surgical Options
Surgery is reserved for chronic fissures unresponsive to conservative and medical treatments.
- Lateral Internal Sphincterotomy: The most common procedure involves cutting a small portion of the internal sphincter muscle to relieve spasm and promote healing. It boasts high success rates but carries risks such as incontinence.
- Fissurectomy: Removal of the fissure edges to stimulate healing.
- Advancement Flap Procedures: Used in complex or recurrent cases, this technique covers the fissure with healthy tissue.
Preventing Recurrence: Long-Term Strategies
Prevention focuses on maintaining healthy bowel habits and minimizing risk factors:
- Maintain a high-fiber diet and adequate hydration.
- Exercise regularly to promote bowel motility.
- Avoid prolonged sitting and straining during bowel movements.
- Manage underlying conditions such as inflammatory bowel disease.
- Seek early treatment for symptoms to prevent chronicity.
Integrating Expert Insights and Patient Experiences
While clinical guidelines provide a framework, individual experiences vary widely. Patients often report that combining dietary changes with warm sitz baths and topical treatments yields the best results. Some find that mindfulness and relaxation techniques help reduce sphincter spasm triggered by stress.
Potential augmentation: Incorporating proprietary patient survey data on treatment outcomes or expert interviews with colorectal specialists could deepen authenticity and authority.
Addressing Common Misconceptions
- “Anal fissures always require surgery.” Most fissures heal with conservative care.
- “Only constipation causes fissures.” Diarrhea and other factors also contribute.
- “Pain means cancer.” While pain is distressing, fissures are benign and treatable.
Actionable Takeaways
- Prioritize a fiber-rich diet and hydration to maintain soft stools.
- Use warm sitz baths regularly to ease pain and promote healing.
- Avoid straining and prolonged toilet sitting.
- Consult a healthcare provider if symptoms persist beyond two weeks.
- Explore medical treatments if conservative measures fail.
- Consider surgery only as a last resort under expert guidance.
Conclusion
Anal fissures, while often painful and distressing, are manageable with a nuanced understanding of their causes and a tailored treatment approach. By combining lifestyle modifications, medical therapies, and, when necessary, surgical intervention, individuals can achieve lasting relief and prevent recurrence. Empowered with expert knowledge and practical wisdom, readers can navigate this condition with confidence and dignity.